Table of Contents
Introduction
Its unlikely that you have ever heard of von Willebrand’s Disease. But, reading this post you will soon realize how common this “unheard” disease is and why it’s important to be aware about the same.
If a thorn pricks your finger and blood oozes out, the natural reaction would be to wince at the slight pain and the forget about the incidence. You instinctively know that this blood will soon stop oozing within few minutes and the wound will heal automatically. This is true for most of us. We are born with mechanisms that easily clot blood oozing from any wound. But there are few out there who are unfortunate and are not born with such efficient clotting mechanism. For these unfortunate souls bleeding doesn’t stop easily. Even a small injury is a matter of grave concern for such patients. One can bleed to death. These patients suffer from what we call as inherited bleeding disorders. Inherited bleeding disorders are genetic diseases that affect the clotting of blood and can result in excessive bleeding inside and outside of the body. Every year around 300,000 people globally get diagnosed with one or the other inherited bleeding disorder. When one hears about bleeding disorder, hemophilia is what most resonate with. However, hemophilia is not the most common one. The most commonly inherited bleeding disorder goes by the name von Willebrand’s Disease (vWD).
In this article we will try to understand what really happens in patients who suffer from vWD. We will discuss complex scientific topics in simple layman’s language, to decrypt the mechanism behind vWD and understand how it can be treated.
World Hemophilia Day- An Awareness Drive
Most of the inherited diseases can’t be completely treated (as of now). Early diagnosis and initiation of treatment is critical for such patients- else the damage caused by such inherited diseases can be irreversible and fatal. Most of the treatment modalities are life- long and work best when initiated at a very early stage. Unfortunately, compared to other diseases genetic diseases get diagnosed pretty late. This is generally because of lack of awareness. Compared to other diseases, in general, clinicians don’t efficiently diagnose genetic diseases and their knowledge about treatment modalities is fairly limited.
Since 1989, every year, 17th April is celebrated as World Hemophilia Day. It is an international initiative that aims at raising public awareness regarding bleeding disorders. On this day, the whole bleeding disorders community comes together to celebrate the continuous advances in treatment of bleeding disorders.
Although named as World Hemophilia Day, we know that the most common inherited bleeding disorder is actually von Willebrand’ s disease (vWD). vWD affects 0.1% to 1% of the total population across the world. On 17th April 2021, the hemophilia community will celebrate 95th anniversary of the first description of von Willebrand’ s disease (VWD) by Dr Erik von Willebrand.
The Pipeline Through Which Blood Flows
In our body blood flows through a complex system of pipes. These pipes originate from the heart as arteries. Arteries carry the blood from the heart to various organs and tissues. As an artery approaches any tissue it keeps becoming narrower and narrower- an artery becomes the narrower “arteriole” which then become the narrowest “capillaries”. Capillaries are narrowest and thinnest- this allows smooth exchange of gases, nutrients and wastes between blood and the tissues. Capillaries take the blood to the wide “venules” which then become the wider “veins”. Veins take the blood back to the heart.

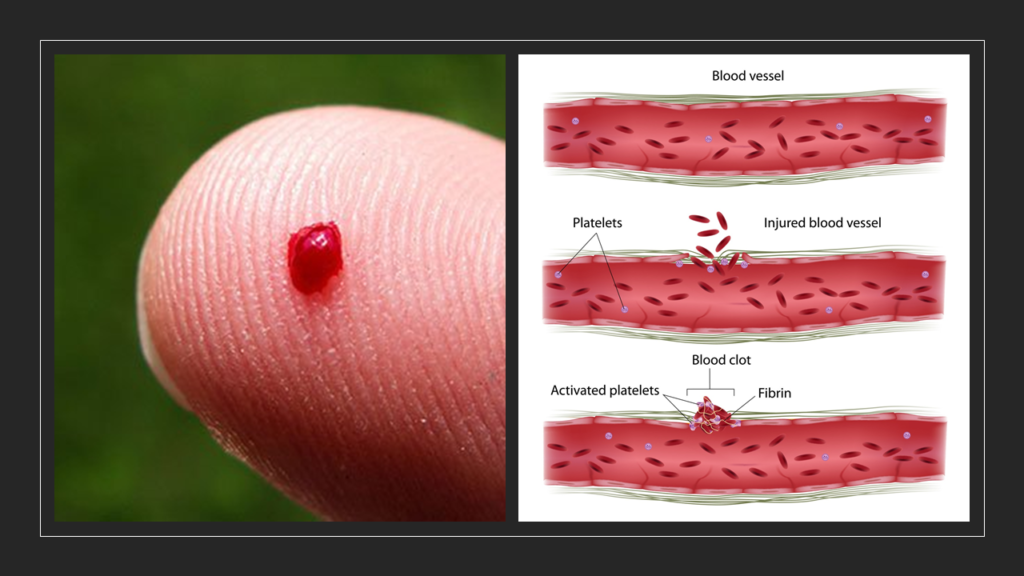
In this entire journey, the integrity of pipelines (arteries, arterioles, capillaries, venules, veins) is critically important. There shouldn’t be any leakages. And this responsibility majorly lies with platelets. Platelets are an important component of blood. They keep swimming within blood keeping a vigilant eye on the pipeline. They can be called as the plumbers of our blood flow system. Although, I must mention that such description severely limits description of the extent of work done by the platelets. For example, platelets are also extremely important components of our body’s system. However, for this post, we will imagine platelets as plumbers swimming inside blood!

The Plumbers And The Adhesives
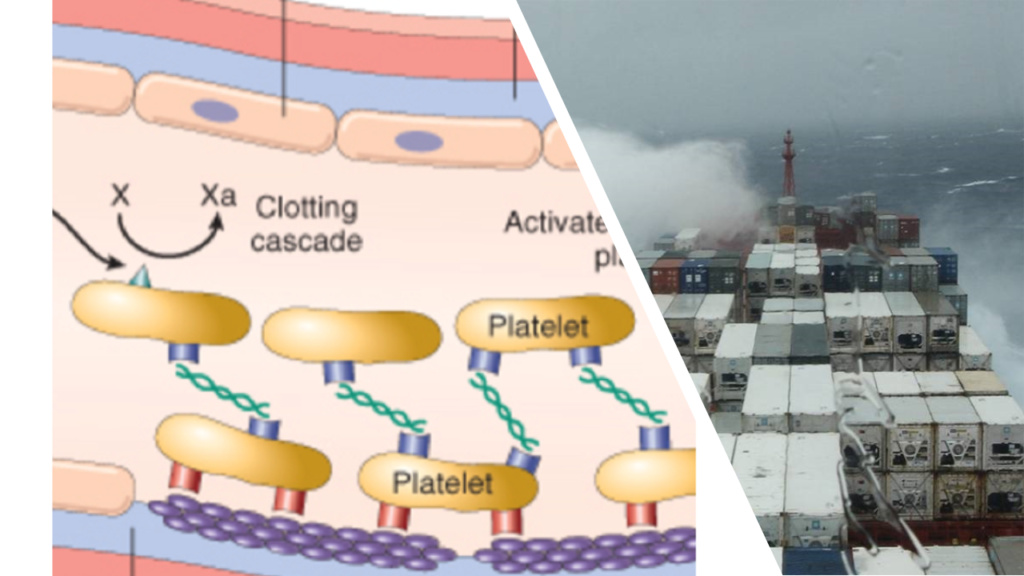
Every second, blood is gushing with a force and rapidity that is bound to cause stress on the linings on the blood vessels and cause injury. Such injuries, if unattended, will lead to leakages in the plumbing system resulting in bleeding. This is why platelets in blood exist. Whenever there is any internal damage, at any part of a blood vessel due to any reason, platelets swing into action immediately. They quickly swim and gather at the site of damage. Then, using a set of adhesives known as “clotting factors” and several other chemicals, platelets orchestrate a complex series of reactions. Finally, a “clot” is formed. Clot acts as tight sealant. It seals up the leak and gives time for underlying damage to heal completely in the due course of time.
Till date we know of 12 different clotting factors which are required for ensuring clot formation. Adequate and accurate levels of each factor is critical for the blood to flow normally. And these levels depend on situation and there is always an accurate balance maintained as per the requirement. Let’s take the example of factor no. 8 (FVIII). FVIII is one of the most important clotting factors. If FVIII levels are unnecessarily low, clot formation is impaired and will lead to excessive bleeding. If FVIII levels are high without any need for such high levels, clot formation is promoted and can lead to unnecessary complications such as stroke, heart attacks etc.
Von Willebrand Factor- A Powerful “Cargo Ship”
FVIII is extremely fragile. The sea of blood contains numerous chemicals that can easily destroy FVIII. FVIII needs a carrier that can protect and transport it safely. Hence, just to carry FVIII, there are special “cargo ships” for it. Each such cargo ship is known as “Von Willebrand Factor (vWF)”. Wherever in the pipeline any damage is detected, these cargo ships unload the FVIII they carry at the site of damage. FVIII, along with other adhesives and chemicals, then participates in the repair work.
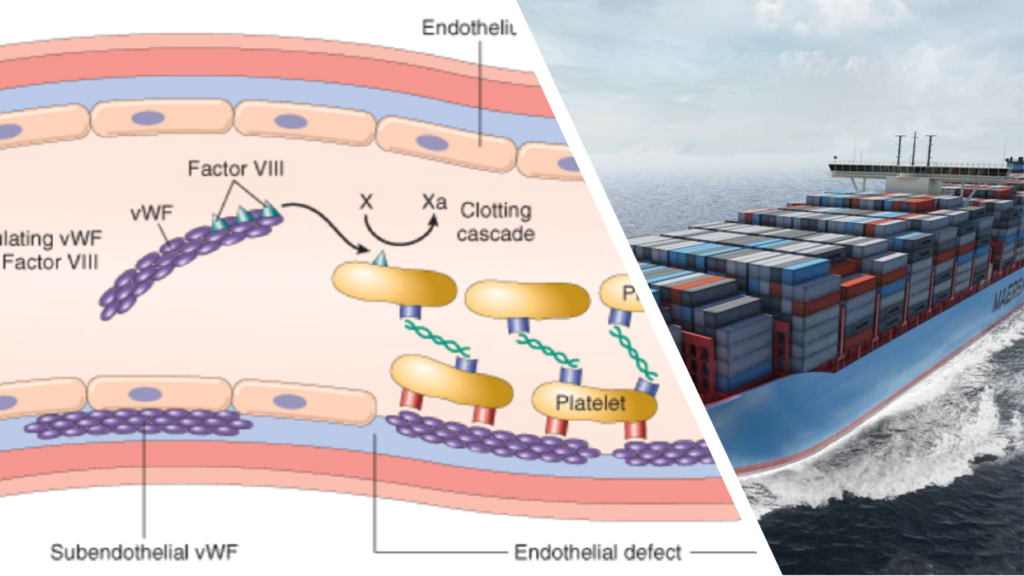
It’s easy to now follow that more the number of such cargo ships, more will be the quantity of FVIII flowing in blood. Since damage keeps happening at multiple locations within the pipeline network of blood vessels, low levels of vWF will lead to bleeding disorder. With the same logic, very high levels of vWF will ultimately make the blood system very sensitive- the plumbers will start reacting to even to insignificant damages. This can cause unnecessary clotting that can trigger thrombo-embolic diseases causing strokes, heart attacks etc. So, both low and high levels of vWF are dangerous. Normal healthy human body maintains an accurate balance such that vWF levels are exactly as required- not more, not less.
The Physics Of “Gush Of Blood”
When blood flows through the pipeline of blood vessels, the entire system expectedly follows the natural laws of physics. When any liquid flows through any tube, it exerts two types pressure on the walls of the tube. The first type of pressure is perpendicular to the wall of the tube, and risks bursting of tube if tube is weak enough. This perpendicular pressure is known as “tensile stress”. The other type of pressure is parallel to the wall of the tube, and risks eroding the inner lining of the tube. This parallel pressure is known as “wall shear stress” (WSS). It should be noted that the tensile stress is much larger in magnitude than the WSS. And hence, our blood vessels have evolved to ensure tensile stress is easily taken care of. The walls of the blood vessels are extremely strong and tensile stress enforced by the flowing blood is most often incapable of causing any damage.
The seemingly weak “wall shear stress” (WSS) is the one that can easily cause damage. This is because WSS creates a pressure that is similar to a kid trying of erode the paint from a wall using her fingernails. As the blood flows, it continuously brushes through the inside of blood vessels. The inner lining of the blood vessels can be easily eroded by the frictional force of high WSS.
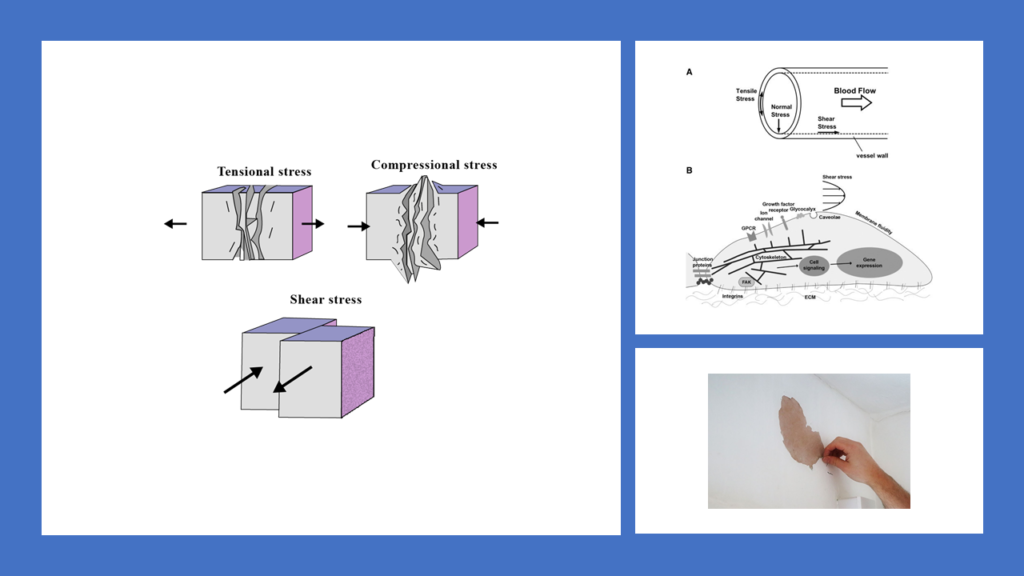
[FOR GEEKS: In terms of physics, WSS can be defined as the tangential stress on the endothelial surface of the arterial wall derived from the friction of the flowing blood. For physics lovers it can be helpful to know that WSS is represented by the symbol τ and is directly proportional to the velocity of blood flow, and inversely proportional to the cube of the arterial radius (R), where flow rate is Q and fluid viscosity is μ.
τ = 4 μ Q/R3]
What this means higher the rate of blood flow, more is WSS; higher the thickness of blood, more is the WSS and lesser the diameter of the blood vessel, more is WSS. Of these three, as obvious from the equation, diameter of the blood vessel is the most sensitive variable. A little decrease in blood vessel’s diameter significantly increases “wall shear stress” (WSS).
High “Wall Shear Stress” (WSS)- Where The Plumbers Can’t Swim!
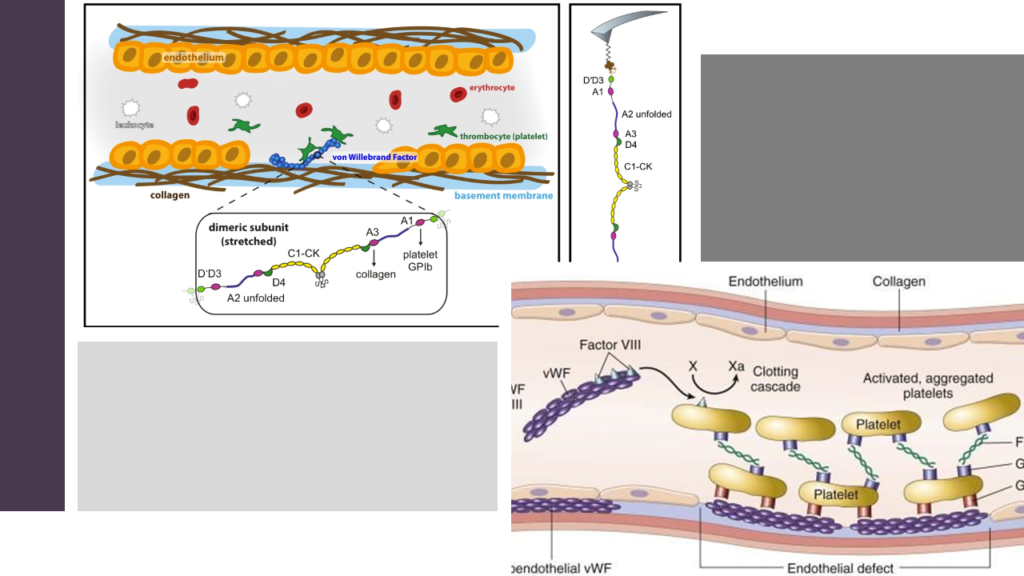
Across the body, the diameters of blood vessels are highly variable. Previously we saw that arteries become continuously narrower as they move away from the heart. Hence, there are several locations across this pipeline of blood vessels where “wall shear stress” (WSS) is much higher than other locations. Naturally, the chances of damage are highest in these locations since frictional forces are very high in magnitude. But then, this is exactly the same reason why “plumbers” of our blood (the platelets) might find it most difficult to repair the damage in these locations. I told you to imagine platelets as plumbers swimming in the blood. At the locations where “wall shear stress” (WSS) is high, the force of the blood gushing against the inner lining of the pipeline is very high. This intense “gush” makes it very difficult for the “swimming plumbers” to float at one place and cling to the site of damage so that they can do the repairs.

So, in these high WSS sites where the gush of the blood flow is very forceful, the plumbers cannot really swim and do their work efficiently. Here, they need powerful ships upon which they can climb and remain at the site of damage in a stable manner.
Earlier we discussed about a container ship called vWF (Von Willebrand Factor) that carries the fragile FVIII safely to locations where plumbers need to use it as adhesive. This same container ship happens to be powerful enough to remain afloat with enormous stability even at locations where WSS is very high. So, whenever there is any damage in the pipeline where WSS is very high and its impossible for the plumbers to swim efficiently, they take help of this container ship. vWF is a very flexible “container ship” that can change its structure adapting proportionately to the force of blood flowing, thus giving the required stability for the platelets to do their job of repairing.
von Willebrand’s Disease (vWD)
Brief Introduction
When body is not able prepare adequate levels of vWF or if vWF that is produced is defective in nature, it will lead to a bleeding disorder. This bleeding disorder, caused due to issues with quantity/quality of vWF, is known as Von Willebrand’s Disease (vWD). In vWD the defect lies in the genes. Hence vWD is known as a genetic disease. It passes from one generation to the other.
Defects in vWF can result in dysfunctional clotting leading to bleeding from gums and other parts of the body. Such bleeding, once it starts, will be prolonged. The impact on patient experiencing such can be mild to extremely severely, sometimes causing death.
Discovery of von Willebrand’s Disease
Hjördis Sundblom was the 9th of 11 children of a family from Foglo. Halfway between mainland Finland and Sweden lies an archipelago of 6,000 islands, known as the Aland Islands (pronounced “Or-land”). Foglo is one amongst these 6000 islands.
Hjördis was suffering from a severe bleeding condition. She experienced regular bleeding from the nose, lips, gums and skin. In 1924, 5 years old Hjördis was brought to Helsinki to seek treatment from Dr Erik von Willebrand. Dr von Willebrand soon discovered that this bleeding condition that Hjördis was suffering from, was familial. Six of her siblings had similar complaints and they all suffered from the same bleeding condition. Three of her sisters had actually died due to complications arising from this bleeding disorder.
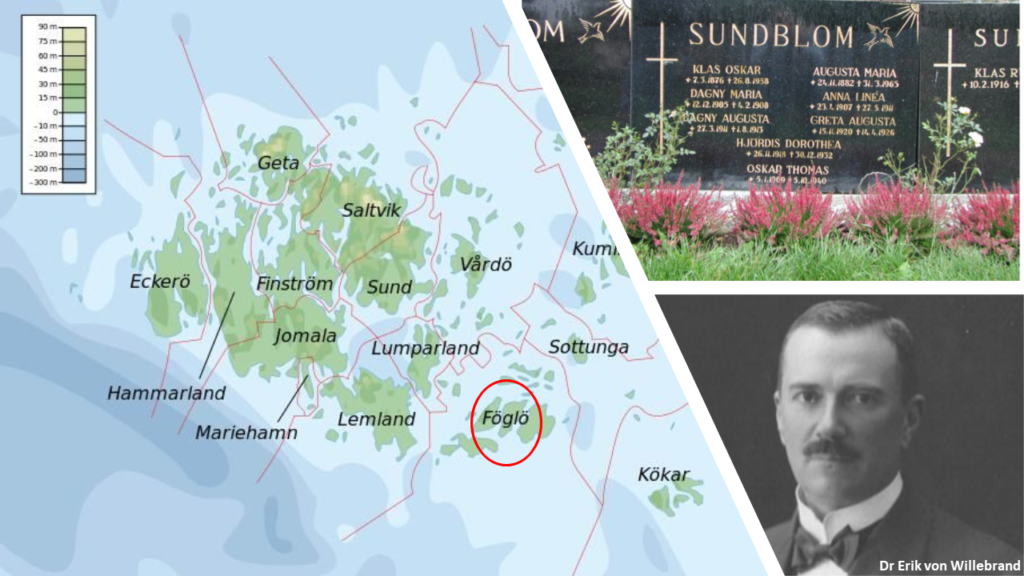
The disease was quite unique, as Dr von Willebrand found. It was nothing like hemophilia, another bleeding disorder that was well known to the doctors then. Hemophilia is also a bleeding disorder and is genetic in nature. But hemophilia generally affects males. Females rarely suffer from hemophilia, and even if they do it usually mild. But, in this family, Dr von Willebrand was astonished to see that the bleeding condition spared no gender. When he did a detailed analysis of the entire family he found that the condition was present in the three previous generations, on both sides of Hjördis’ family. 16 of the 35 women analyzed had the disorder that Hjördis was suffering with. Similarly, 7 of the 31 men he analyzed had the same bleeding condition. These observations led Dr von Willebrand conclude that unlike hemophilia, which is X linked genetic disorder, this condition is autosomal dominant. Please don’t get bogged down by the usage of such medical terminologies- we will discuss these terminologies soon.
In 1926 Dr Erik von Willebrand published an article in Swedish about this new disease. The article was titled “Hereditär pseudohemofili” (“Hereditary pseudohemophilia”). But he couldn’t find any appropriate treatment. 4 years later, in 1930, Hjördis bled to death. In 1931 this new bleeding disorder came to the attention of the world when German language version “Hereditär pseudohemofili” got published. It came to be called as von Willebrand’s Disease after its discoverer.
What happens in von Willebrand’s Disease?
Since the discovery of von Willebrand’s Disease, lot of research has happened. In 1971 von Willebrand Factor (vWF) was discovered. Now scientists finally knew what happens in von Willebrand’s Disease (vWD). Due to a genetic defect, there is defective production of vWF. Quantity or quality or both can get impacted. Either ways, there is not enough healthy vWF to do perform the assigned functions efficiently. We saw that vWF can be imagined as cargo ships in our blood that carry FVIII. Lack of sufficient number of good quality cargo ships means FVIII now cannot be carried and delivered in required amounts. FVIII is a critical adhesive required for clot formation, without which the plumbers in the blood are now handicapped. These plumbers can no longer repair the constant damage that keeps happening along the inner lining of the blood vessels. At the locations of high WSS (wall shear stress) the situation becomes grim. These are the locations which get damaged more frequently and these are the locations where the plumbers cannot swim efficiently- they need support of vWF. Without enough high quality vWF, high WSS locations suffer twice- first the plumbers can’t reach and gather properly to repair, and even if they manage somehow the adhesives won’t work because there is not enough FVIII.

Types of von Willebrand’s Disease
We now know that this disease can exist as either of the three main types. In type 1 there is partial quantitative deficiency of vWF. In type 2 the problem is with the quality of vWF- it’s structurally defective and is inefficient in doing its functions. Type 2 vWD is further divided in several subtypes (including types 2A, 2B, 2M and 2N), each of which is associated with a specific functional or structural defect. Type 3 is the most severe one where there is complete deficiency of vWF.
| vWD Type | Frequency (% of vWD) | Impact on vWF | Severity |
| 1 | 70% | Partial quantitiative deficiency | Mild to severe |
| 2A | 10-15% | Qualitatively defective vWF | Moderate to severe |
| 2B | <5% | Qualitatively defective vWF | Moderate to severe |
| 2M | <10% | Qualitatively defective vWF | Significant |
| 2N | Uncommon | Qualitatively defective vWF | Mild to moderate |
| 3 | Common in scandinavian countries; else very rare | Virtually complete quantitiative deficiency | Very severe |
Genetics of von Willebrand’s Disease
(You may want to read the genetics section my post on “Gotra System” to get a brief understanding of genetics)
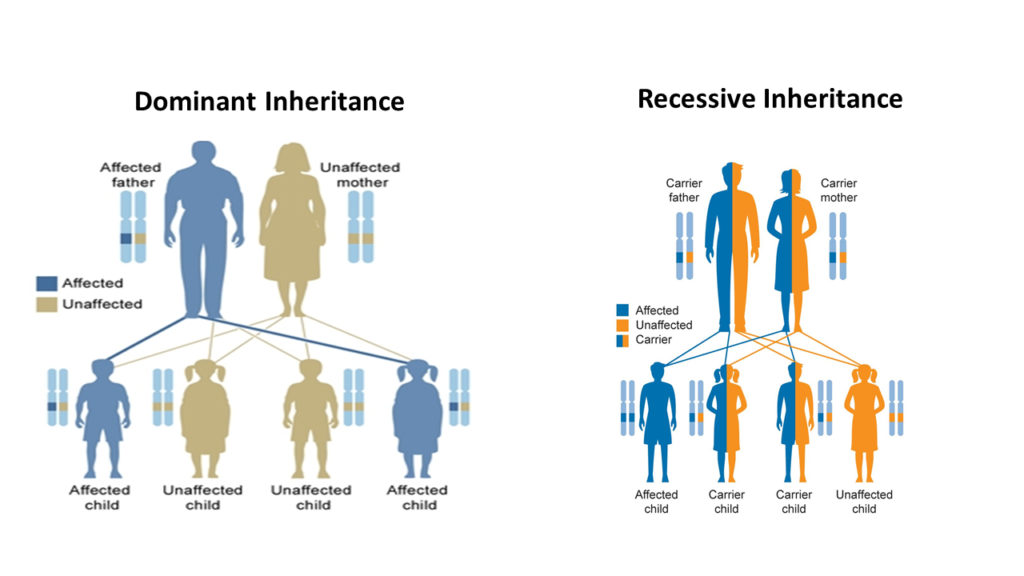
In a cell that prepares vWF, the recipe for preparing vWF is located in a gene on chromosome 12. This gene is known as vWF gene. If the defect in this gene that causes vWD. Since it is not on the sex chromosome (X or Y), it occurs equally in men and women. Types 1, 2A, 2B, and 2M affect in a dominant fashion. Type 2N and Type 3 VWD have a recessive inheritance pattern.
You may find these terms (dominant, recessive etc) confusing. While I will be soon writing a detailed post explaining these later, let me briefly make you understand. Chromosomes exist in pairs. So every person will have 2 Chromosome 12s- each having 1 vWF gene. Thus, there are 2 vWF genes. If 1 vWF gene is defective, the other copy can be used to prepare vWF.
Sometimes, the defect is so gross that just 1 defective gene is enough to cause the damage- the other gene, even if normal, cannot come for rescue. Such a “strong” defective gene is then called as “dominant”. This is what I mean when I say Types 1, 2A, 2B, and 2M affect in a dominant fashion. In these types of vWD, the patient suffers from bleeding disorder even if he/she has defect in just one copy of the gene.
However, in few cases the defective gene might not be so dominant. If the other gene copy is normal, it can easily mask the defect of such “non- dominant” gene. Such a “weak” defective gene is known as recessive. In such recessive genetic diseases, a person carrying just one copy of defective gene won’t suffer. He/she will only “carry”, but will not suffer. Hence, they are known as carriers. In recessive genetic diseases, the disease is mostly seen in only those unfortunate ones who have defects on both the copies of genes. Type 2N and Type 3 VWD are recessive and in these types of vWD patient suffers from bleeding disorder only if he/she has defect in both the copies of the gene. Sometime even Type 2A can behave as recessive.
The expression of vWF varies from patient to patient (we call this as “penetrance” and “expressivity”). Hence in many patients there is mild deficiency of vWF. Such patients often remain asymptomatic and are only diagnosed if testing is performed as a part of genetic screening if a relative has symptomatic disease
| vWD Type | Inheritance pattern |
| 1 | Autosomal dominant |
| 2A | Autosomal dominant/ recessive |
| 2B | Autosomal dominant |
| 2M | Autosomal dominant |
| 2N | Autosomal recessive |
| 3 | Autosomal recessive |
Biomechanics of FVIII, vWF and vWD (Only for the Geeks)
Till now, I have been discussing about platelets, clotting factors and vWF using simple analogies so that any layman can visualize what’s really going on. But few geeks might be interested in knowing the complex molecular mechanisms of vWF.
vWF is a multimeric glycoprotein. It circulates in plasma at a concentration of 5–10 μg/ml. vWF is also present in platelet α-granules, in Weibel-Palade bodies of endothelial cells, and in the subendothelium.
Coagulation factor VIII is highly volatile and is susceptible to rapid destruction when left exposed on its own in blood. vWF serves as a carrier protein for coagulation factor VIII protecting it from such premature destruction. vWF circulates together with FVIII in the plasma as a loosely coiled protein complex. Under normal conditions, this protein complex does not interact with platelets or endothelial cells. However, when a blood vessel is injured, vWF binds at the sites of injury by adhering to the exposed subendothelial structures including collagen. Bound vWF then grab platelets from the flowing blood, especially under high shear stress conditions. This results in platelet activation and aggregation and finally thrombus formation. Thus, vWF acts as a molecular bridge between platelets and exposed components of the sub- endothelium and this molecular bridge is used to build the platelet thrombus. The role of VWF is particularly important at locations where WSS is very high- in such locations vWF is the only molecule able to promote platelet adhesion and platelet aggregation in a flow-resistant manner. This is because vWF is a rather unique molecule in its ability to change shape according to type of flow.
Treatment of von Willebrand’s Disease
History
By 1950s it became known that in vWD patients FVIII was decreased and that transfusing plasma fractions derived from healthy donors could be helpful in treatment. The first human plasma-derived concentrates of FVIII were introduced in the 1960s and transformed the lives of such patients. During those days, the FVIII concentrates were obtained by pooling large quantities of human fresh-frozen plasma preparations. But this process involved considerable risk of transmitting viral diseases. It was impossible to screen all donors for all viruses they harbor, and there was huge possibility that fresh-frozen plasma sourced from these donors might contain viruses
It was the German scientist, Professor Heimburger, who took this problem very seriously and found very effective way to inactivate viruses in plasma preparations. This research eventually, in the late 1970s, led to the development of Haemate P. Hemate P became the first effectively virus inactivated FVIII plasma product, and has been available in the market since 1981.
Management Strategies
The management of vWD generally involves the use either or combination of three strategies:
- Stimulate production and release of vWF from body cells
- Replace vWF from outside
- Promote clot formation and wound healing.
Desmopressin
In our body vWF is produced by platelets and endothelial cells (the inner lining of blood vessels is known as endothelium). Desmopressin is a chemical that excites the platelets and endothelial cell to release vWF. Hence Desmopressin is routinely used for treating vWD. However, one must remember that for Desmopressin to work, there must be some amount of vWF produced inside these platelets and endothelial cells. Hence in severe cases of Type 1 vWD (where vWF produced is too scanty) and in Type 3 vWD (where vWF is not produced at all), Desmopressin will not be helpful. In vWD types 2A and 2M, Desmopressin does work- but the effects are not upto the mark since the quality of vWF that is produced is too bad. In vWD type 2B, the quality of vWF is so bad that excessive release of such defective vWF can be injurious. Hence Desmopressin is contraindicated in patients with vWD Type 2B.
Desmopressin works best for patients with Type 1 vWD of mild to moderate severity. In such patients, there is decreased production of vWF- but not too low and Desmopressin works like a charm. A 30 minutes intravenous infusion of desmopressin in such patients leads to 3- to 5-fold increase in vWF levels within 60 minutes. Consequently, even FVIII levels increase.
| vWD Type | Response to Desmopressin |
| 1 | Good |
| 2A | Mild to moderate |
| 2B | Containdicated |
| 2M | Mild to moderate |
| 2N | Sub- optimal |
| 3 | No response |
Problem with Desmopressin is that the effect is not long lasting. High vWF levels are generally maintained for only 6 to 8 hours post Desmopressin use. Treatment with Desmopressin must be repeated every 12 to 24 hours, depending on the type and the severity of the bleeding. Such frequent usage leads to another issue- body stops responding to Desmopressin.
The main advantages of Desmopressin are its low cost, ready availability, and ease of use. It is preferred over plasma concentrates whenever possible as the plasma concentrates theoretically can transmit blood-borne infections.
A drug that has effects will also have side effects. So is true with Desmopressin. Desmopressin may increase heart rate (known as tachycardia), cause headache and facial flushing. It can lead on fall in blood sodium (known as hyponatremia), particularly in children. Some experts have claimed use of Desmopressin causing thrombosis, heart attack and stroke- but these are extremely rare.
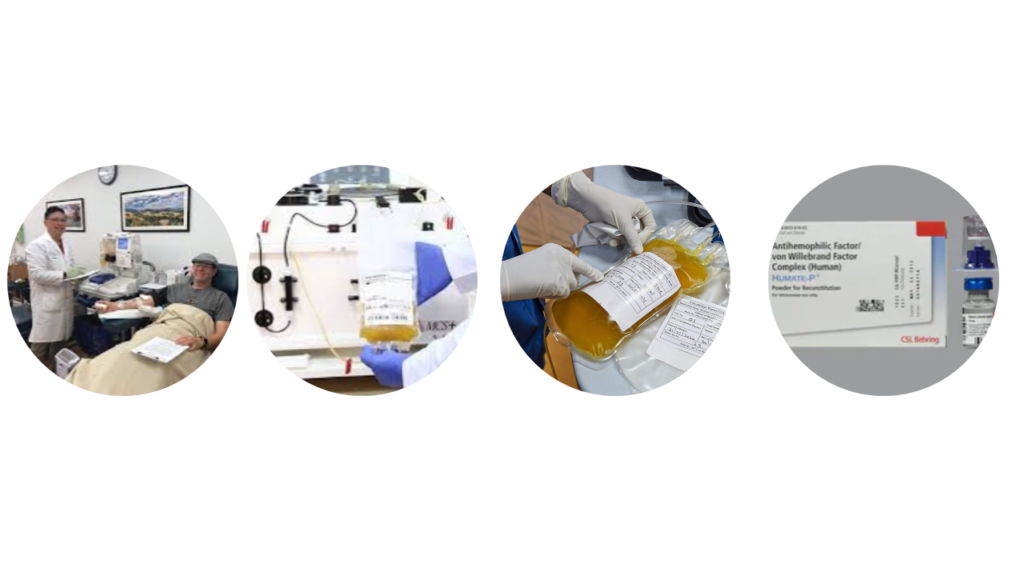
Plasma Derived Products
vWD patients, who respond unsatisfactorily to Desmopressin, have to be treated with transfusion therapy using vWF products manufactured from pooled human plasma. Here, it is important to remember that in vWD even FVIII levels go down. Bleeding can be controlled only when, vWD and FVIII, both are in adequate quantity. If you use a plasma concentrate that contains just vWF and not FVIII, it might not work in severe cases such as Type 3 vWD. In Type 3 vWD if you use plasma concentrate containing just vWF and not FVIII, it will take almost 6- 10 hours post infusion for FVIII levels to rise normal. And this will be too late if there is an ongoing bleed. Hence, its important to ensure vWF and FVIII levels are brought to normal simultaneously.
Today there are plasma concentrates available in the market that contain both vWF and FVIII. This has really improved lives of patients with vWD. For example, Haemate P (we already talked about Haemate P earlier) contains the vWF/FVIII-complex. It has been used since past 40 years now with excellent efficacy and safety and tolerability. During this long clinical experience with Haemate P, there haven’t been any documented cases of viral transmission.
Recombinant therapies
One of the issue with plasma derived products is that the production is limited to the availability of the donors. The other issue is the risk of viral infections. Although the processes used today are extremely refined and efficient compared to earlier days, the risks are still valid.
Recombinant DNA technology has been a revolution tackling such issues. In humans we saw that cells create vWF reading the recipe coded by the gene in chromosome 12. The vWF thus produced is then released into plasma. It is this plasma, which is collected from the donors to treat the unfortunate ones suffering from vWD.
Recombinant DNA technology mimics what a human cell does, in a large manufacturing units known as bioreactors. The concept is simple. A cell is a cell and produces what is written in the gene. So, even if a bacterial cell is made to read normal vWF gene it will product normal vWD. It is easy to produce huge quantities of vWF using such methodology, without relying on any donor and completely mitigating the risk if viral infections. Also, the vWF produced in such a way will be of very high quality because all the gene “recipe” is under manufacturer’s control.
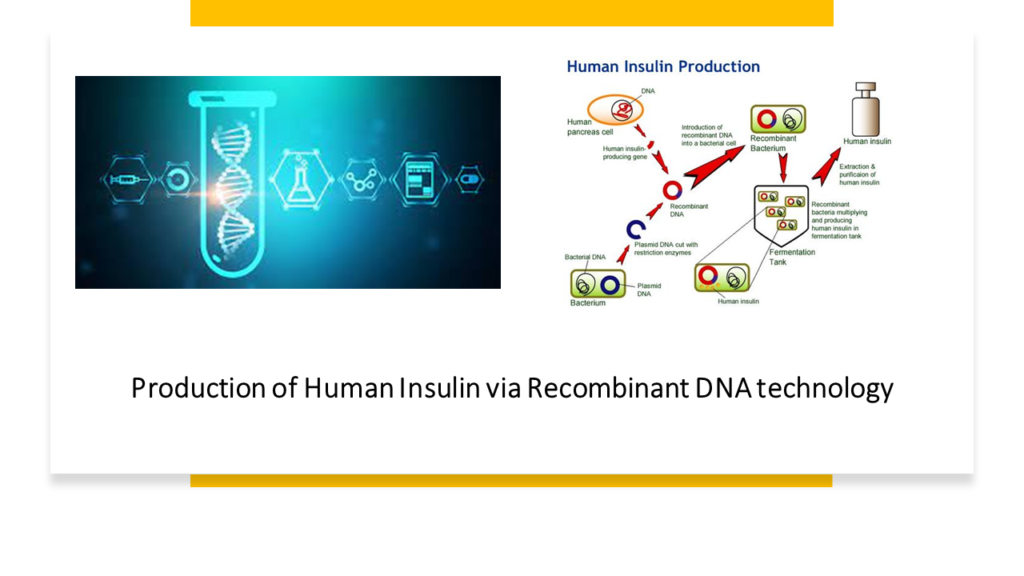
Recombinant vWF has recently been approved in the United States and has been shown to be extremely effective in managing vWD. The current bioreactors producing recombinant vWF use animal cells called Chinese Hamster Ovary (CHO) cells to read the vWF gene and produce vWF artificially. One issue is that the recombinant VWF preparation does not contain FVIII. Therefore, most patients will require concomitant administration of FVIII along with the initial dose of recombinant VWF.
Acquired von Willebrand Syndrome (AvWS)
In few patients with vWD, there is no genetic defect in the vWF gene on chromosome 12. But vWD levels are nevertheless low. Such cases on vWD are known as acquired vWD. Acquired vWD is also known as Acquired von Willebrand Syndrome (AvWS). In most of such cases, the platelets and the endothelial cells produce vWF normally. But then the vWF gets destroyed because of toxic elements resulting from some other disease. AvWS can be seen in patients suffering from cancers, cardiovascular diseases, autoimmune diseases etc.
AvWS was described for the first time in 1968, in a 7-year-old boy suffering from another disease called SLE (systemic lupus erythematosus).
Final Note
On 17th April when we celebrate World Hemophilia Day we must not get deceived that its only about hemophilia. It’s a day when we pledge for awareness regarding early diagnosis and management of all bleeding disorders. vWD is the most common of these bleeding disorders. And its easy to miss, because several patients don’t show significant symptoms. Significant progress has been made in our understanding of vWD since it was first described in 1926 by Dr. Erik von Willebrand. Today medical science has progressed enormously. Kids like Hjördis Sundblom and her sisters, who have bled to death due to vWD, may not suffer such horrendous outcomes today; they now have a very good chance of living a normal life.



Looking forward to reading more. Great blog article. Thanks – Again. 189433419
Glad that you liked it!
I think, what is it good idea.
I think, that is not present.
You have hit the mark. I think, what is it excellent thought.
Very useful piece
Yes, really. All above told the truth.
https://how-tonow.fun/map.php
Thank you! I am glad that you found this article useful.
Von Willebrand’s disease is a bleeding disorder. When you have this disease, it takes longer for your blood to form clots, so you bleed for a longer time than other people. Normally, when a person begins to bleed, small blood cells called platelets go to the site of the bleeding and clump together to help stop the bleeding.
You are absolutely right!!
What is von Willebrand’s disease? Von Willebrand’s disease is a bleeding disorder. When you have this disease, it takes longer for your blood to form clots, so you bleed for a longer time than other people.
You are absolutely right
Great article! We will be linking to this particularly great post on our website. Keep up the good writing.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
I value the article post.Really looking forward to read more. Cool.