Table of Contents
What will you learn in this article?
Lead is a known poison and lead poisoning is known as plumbism. Lead is highly versatile heavy metal. It is non-degradable. Lead easily gets accumulated in the body and remains undetected for a very long time, makes it a serious environmental health hazard. Medical science has proven that lead affects almost every part of the human body. Lead has irreversible effects on neurobiological development of young children and fetus, and its poisoning has lasting implications on the human life.
Lead is universally present, thanks to industrialization. It’s very easy for any of us to get exposed to this killer unknowingly. Many keep suffering from complications of plumbism for years, not really suspecting that its lead that is poisoning their lives.
Hence, its critical for each one of us to be aware of this poison and protect us and our families from plumbism. This is the aim of my current post. In this post I would be outlining the symptoms, diagnosis, and treatment therapy for lead poisoning. This will be a detailed post that can used as reference by readers to drive a better understanding of the science entailing lead poisoning. Although this topic must be dealt with detailed science, I will try my best to keep explanations simple enough for even a layman to understand.This article offers free shipping on qualified Face mask products, http://fakewatch.is or buy online and pick up in store today at Medical Department
Lead- A Metal of Antiquity
Since prehistoric times (till 13th century AD), humans had identified 7 metals that were used extensively. These 7 metals- lead, gold, silver, copper, tin, lead, iron, and mercury- were known as the metals of antiquity.

The 7 metals of antiquity were so valued by human civilizations that they were incorporated in various mythologies and were used for religious symbolisms. Alchemists and astrologers assigned planets and days to these 7 metals of antiquity. Universally silver was always associated with the Moon, and gold was always associated with the Sun. Iron, used always for making weapons, was associated with Mars. The soft, pliable metal copper was linked with Venus, and the chameleon like metal mercury had the same name as its planet.
| Metal | Planet | Day of week |
| Gold | Sun | Sunday |
| Silver | Moon | Monday |
| Iron | Mars | Tuesday |
| Mercury | Mercury | Wednesday |
| Tin | Jupiter | Thursday |
| Copper | Venus | Friday |
| Lead | Saturn | Saturday |
Lead- An Omnipresent Poison
So, lead was always a widely used metal since prehistoric times. For 6000 years man has been extensively using lead owing to its versatile properties such as malleability, ductility, poor conductibility, softness and resistance to corrosion. Lead has wide industrial and household applicability due to its obvious physiochemical properties, low cost and easy workability. Hence lead finds its use in over 900 occupations including smelting, mining, battery manufacturing etc.
Needless to say, such widespread usage of lead for so many thousands of years has resulted in its wide distribution in the environment. Its very easy to find lead enter human body through various sources- many of them are so common and uninspiring that most of us will never suspect these sources to be the ones releasing lead into our body. Lead is non-biodegradable and body finds it very difficult to eliminate lead. Because of this, lead tends to accumulate in body. Accumulation of even small quantities of lead leads lead poisoning. Lead poising, also known as plumbism, is extremely dangerous and lethal. And it is common.
Dangers of lead poisoning has been known since ancient times. Hippocrates described a case of severe colic possibly due to lead poisoning way back in 370 BC. In the 2nd century BC Nicander described the relationship of constipation, colic, pallor and paralysis to the lead poisoning. Pliny (AD 23–79) talked about lead poisoning in his works. During his times lead workers would tie up their faces in loose bags ‘lest they should inhale the pernicious dust’. Dioscorides (AD 100) knew that intake of lead compounds can cause colic, paralysis and delirium. Later Ramazzini wrote about potters working with lead that ‘at first tremors appear in the hands, soon they are paralysed’.
The earliest record of lead poisoning among white-lead workers in England was probably made by Vernatti in 1678. He noted that the general population could also be exposed to significant amounts of lead due to poorly glazed ceramic ware, the use of lead solder in the canning industry, high levels of lead in drinking water, the use of lead compounds in paint and cosmetics and by deposition on crops and dust from industrial and motor vehicle sources.
In 1823 Benjamin Franklin lost 10 men of his team while trying return from the tragic expedition of the unexplored Hudson Bay. Bones and hairs of these dead men reveal toxic levels of lead deposition. This lead probably entered through the meat that was stored in tin cans- these tin cans were soldered and sealed with materials containing high amounts of lead.
Despite this knowledge about lead poisoning since thousands of years and despite the fact that there have been continues awareness campaigns globally since several decades, lead poisoning still continues to affect millions of adults and children worldwide.
How Does This Poison Enter Human Body?
Lead is present in our environment and is considered a pollutant. Lead exists in two forms- inorganic and organic. Inorganic lead consists of lead oxides, metallic lead, and lead salts. Organic lead includes the tetra-alkyl lead compounds mainly tetraethyl lead and tetramethyl lead which have been incorporated into gasoline as anti-knock additives.
Lead can enter human body through food, water, soil and air. For many, lead poisoning is a gift from their occupation that involves regular contact with lead. Such occupational exposure also puts the families of these individuals at risk due to the ‘take home lead’ with their clothes. This is especially true for miners since lead is a metal that is abundantly found in the earth’s crust. Workers involved in occupations such as refining, smelting, battery manufacturing and recycling and car repair etc. are also exposed to lead.

Lead pollution was at peak during the 20th century. One of the most important contributors to this was the rampant use of tetraethyl lead (TEL) across the world. In 1920s General Motors identified TEL as an effective antiknock agent that prevented exhaust valve and valve seat wear. Tetraethyl lead (TEL), when mixed with gasoline, acted as “octane rating booster” that allowed engine compression to be raised substantially. This, in turn, increased vehicle performance and fuel economy. During 1970s usage of TEL in gasoline was at its peak. So wide was its usage that the worldwide production of TEL during 1970s was of the order of 500,000 tonnes. It is believed that the use of leaded gasoline alone deposited close to 4–5 million tonnes of lead in soil, just in the United States. We do not know the extent of such deposition worldwide.
Eventually, usage of TEL in gasoline was banned due to associated hazards to lead poisoning. The current production of TEL has reduced to ~4500 tonnes (which means it’s still produced and used!). In the United States the mean blood lead levels declined from 15.8 to 2.8 μg/dl between 1976 and 1991.
Earlier lead used to be an important component of paints. So, the older buildings, with paint wearing off or those being renovated, generate lead dust and expose the people living in vicinity. PVC pipes used for sanitation and in the potable water supplies use lead as stabilizer. Such usage also poses a threat of lead toxicity due to leaching of lead from the linings.
Several of the Ayurvedic and Chinese medicines contain lead. If used irrationally by an “untrained” practitioner, these medicines can be a source of lead poisoning. Several “innocent” looking items such kajal and surma (used as eye cosmetics in India and Arabic countries) contain lead. And so does cheap toys, which many parents might not even suspect as source of lead poisoning.
In the 1980s, in just a few months, multiple cases of lead poisoning were diagnosed amongst numerous Arabs living in a specific area in Israel. These cases were admitted to Jerusalem hospitals. The source of lead contamination was finally traced to the domestic processing of flour in a particular group of Arab villages.
In 2003 higher levels of lead were detected in certain districts of Washington DC, especially in children. Investigations revealed that a change of disinfectant in the public water supply from chlorine to chloramine led to excessive leaching of lead from the inner lining of the water pipes.
| Occupational Sources of Lead Poisoning Lead mining and refining, plumbing and pipe fitting, auto repair, glass manufacturing, printers, battery manufacturing and recycling, construction work, firing-range, plastic manufacturing and gas stations |
| Environmental Sources of Lead Poisoning Lead paint, soil or dust near roadways, lead-painted homes, plastic window blinds, plumbing, ceramic ware and lead-core candle wicks |
| Other Sources of Lead Poisoning Traditional medicine, gasoline sniffing, costume jewelry, cosmetics, glazed pottery making, target shooting at firing ranges, lead soldering, preparing lead shot or fishing sinkers, stained-glass making, painting and car or boat repair |
Who are more prone to Lead Toxicity?
Amount of lead entering our system depends on the route of entry. In case of adults, if lead is ingested, 20–70% of this lead will find its way into blood.
But almost 100% of the inhaled lead directly gets absorbed into blood.
Absorption of lead is 3 times higher in children compared to adults. Also children retain 30% of lead absorbed compared to 1% in adults. Thus children are more susceptible to lead poisoning. Young children (9 months to 3 years), especially, are most vulnerable groups. This is because of their exploratory behavior. The frequent hand-to-mouth activity of children belonging to this age group is 5 to 10 times more effective in delivering lead into their system. This is also the age of rapid development where lead can have significantly deleterious impact.

The other high-risk groups include occupationally exposed workers and artisans and their families. Similarly, pregnant women along with the growing baby inside womb also have higher risk of lead toxicity. The amount of lead absorption is generally higher for patients having calcium, zinc or iron deficiency.
In the body 95–99% of ingested lead is get collected into the RBCs erythrocytes. From there eventually lead gets transferred to other tissues across the body. Lead usually gets stored in bones and teeth. It also gets deposited in hairs and nails. The rate of deposition of lead in bones and teeth is almost 95% in case of adults while 70% in case of children.
It is important to remember that lead thus deposited in bones and teeth is not always toxic. It is generally the presence of lead in blood that causes toxic effects. But we also need to remember that bones are not static. In children and pregnant women there is significant remodelling of bones. During such remodelling, the lead from the bones and teeth gets released into the blood stream manifesting its toxic effects. And this can happen years after initial exposure. While, half-life of lead in blood is up to 30 days, its storage in bone can remain for more than 20 years. (Half life refers to how much time it takes for a substance to decrease to 50% of its original quantity).
Blood lead level (BLL) a major criteria that is used to measure the extent of the lead poisoning. Another important criterion to measure lead toxicity is ‘body burden of lead’, which calculates the amount of lead which is deposited in the soft tissues and bones of the body. For a large period of time the toxic lead levels had remained undefined. As scientific evidences started accumulating regarding dangers of lead, scientific community’s tolerance for lead kept going down with time. For example, between 1960 and 1990, ‘blood lead level of concern’ were lowered incrementally from 60 to 25 μg/dl. In 1991, it was lowered to 15 μg/dl. Until 2012, Centers for Disease Control (CDC), USA had set toxic BLL to be above 10 μg/dl for all. But in 2012 CDC redefined the standards once again. The BLL was now set at > 10 μg/dl for adults but >5 μg/dl for children.
Diagnosis of Lead Poisoning
In majority cases lead toxicity remains asymptomatic and goes unnoticed. Often most of the symptoms are similar to other disorders. Because of this, most often, lead poisoning remains undiagnosed and untreated. Hence general awareness and education regarding lead toxicity is really important.
In case of children, the BLL needs to be determined along with proper examination to check possible growth retardation, language or speech dysfunction, anaemia and behavioural or attentional disorders.
The primary test in all suspected lead poisoning cases is to estimate the BLL.
Microscopic examination of blood smears may show what is known as “basophilic stipplings” amongst the red blood cells (RBCs). These appear as numerous blue colored dots within the RBCs. Presence of “basophilic stipplings” is considered as diagnostic of lead poisoning in cases where there is already some clinical suspicion of the same. 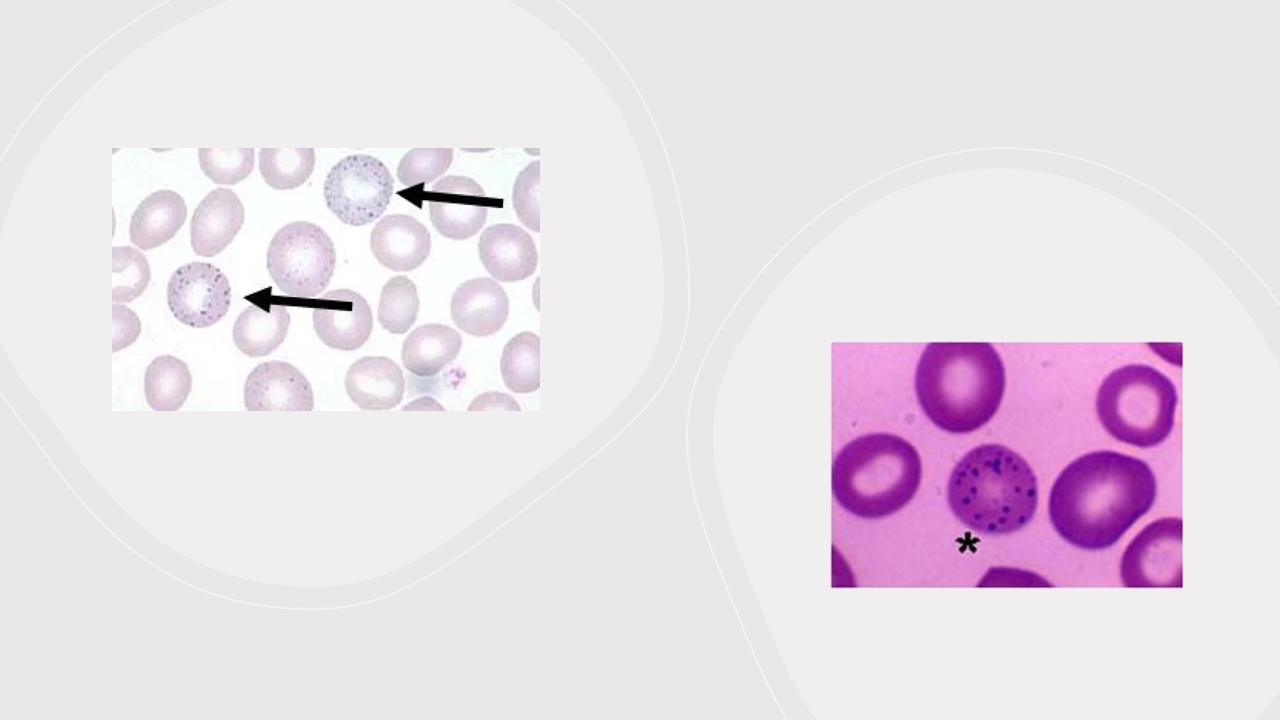
Basophilic stipplings suggest serious injury to bone marrow where RBCs are produced. This bone marrow damage also leads to aberration in the chemical reaction that is necessary for formation of hemoglobin in RBCs. This aberration leads to increased levels of chemicals such as urinary porphyrins, coproporphyrins, zinc protoporphyrin and erythrocyte protoporphyrin(EP).
Clinicians must remember that EP levels solely cannot be used for diagnosis of lead poisoning. EP also rises in iron deficiency which is quite prevalent in developing countries like India.
The same dysfunction in formation of hemoglobin leads to excess of a compound called δ-aminolevulinic acid (ALA).
Increase secretion of ALA in urine is considered as an indicator of lead poisoning.
Patients suffering from long term lead poisoning often experience painful episodes that causes swelling of joints (especially at the big toe). This swelling happens because of deposition of needle shaped crystals of a compound called uric acid that is being excessively formed in lead poisoning. Excess uric acid formation indicates lot of cells are dying rapidly. This gout is also known as “saturnine gout” and has been known since many centuries. The term “saturnine” refers to lead’s association with planet Saturn. During ancient times, lead poisoning was probably common among the upper classes of Roman society. Experts believe that the deaths of some Roman emperors and officials can be attributed to the addition of lead solutions to wine and port. Leaded water pipes were also rampantly used during those times. Skeletal remains of Romans at Cirencester, England, show evidence of gout. “[Many] persons troubled with gout, dropsies and colics and the like…who live upon prepared dainties”– this statement is from an eyewitness account was given by one Musonius (20–90 AD) and refers to gout as being a common disease across during those olden times. It is likely that this “pandemic” of gout resulted from the excessive exposure to lead.

Patients will lead poisoning will have reduced total hemoglobin, low red blood cell count and low thyroid hormones (T3 and T4) while their white blood cell (WBC) count will remain fairly unaffected for a long time. Sudden exposure to high levels of lead (known as “acute” lead poisoning) can cause a devastating anemia called haemolytic anaemia where RBCs start getting killed rapidly. In case of chronic lead poisoning (where there is exposure to lead for over a long period of time), RBCs don’t get killed so rapidly. But these RBCs turn out to be immature with low amount of hemoglobin and with size that is either smaller than normal or normal (Doctors call this as normocytic/microcytic hypochromic anaemia with reticulocytosis).
BLL is good test for screening lead poisoning.
But one must understand that BLL is just an indicator of recent lead exposure. BLL does not reflect upon the total “body burden of lead”.
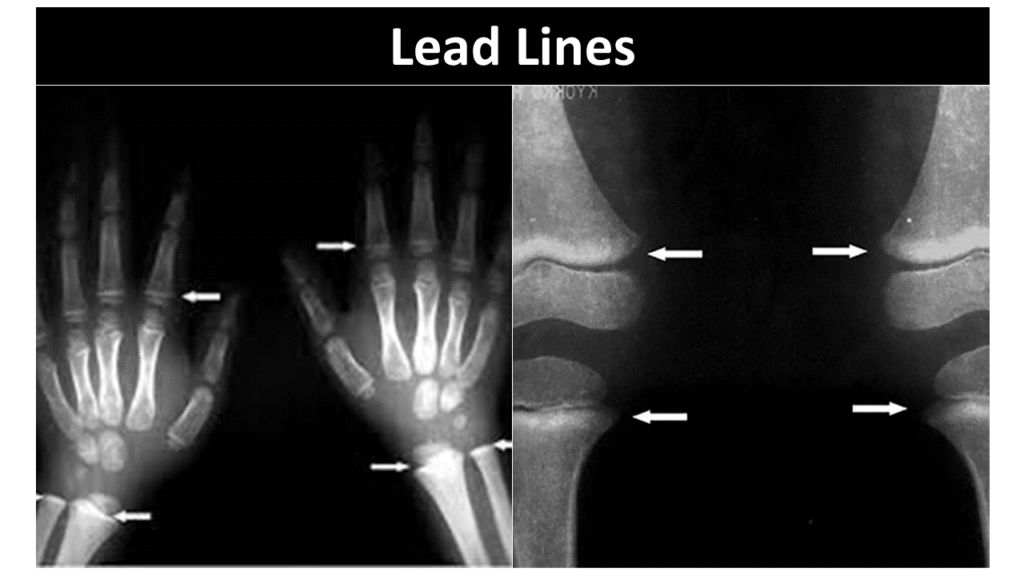
In order to determine the total body burden, doctors generally use a radiological technique involving X-ray fluorescence. This is a non-invasive method to measure whole body lead in bones. Abdominal X- rays often help revealing lead containing foreign materials such as paint chips that have accumulated in the gastrointestinal tract. However, such abdominal X-ray is useful only in cases of acute ingestion of lead or when there unusually long persistence of high BLL. X-rays of long bones such as those of arms (eg. humerus) and thighs (eg. femur) can show “lead lines”. These lines represent increase in density around the “growth” segment of the bone. Their presence indicates growth retardation of the affected bones due to lead poisoning. Although I must mention here that identifying “lead lines” is not a routine procedure to identify lead poisoning. But “lead lines” indicate a definite case of chronic exposure to lead.
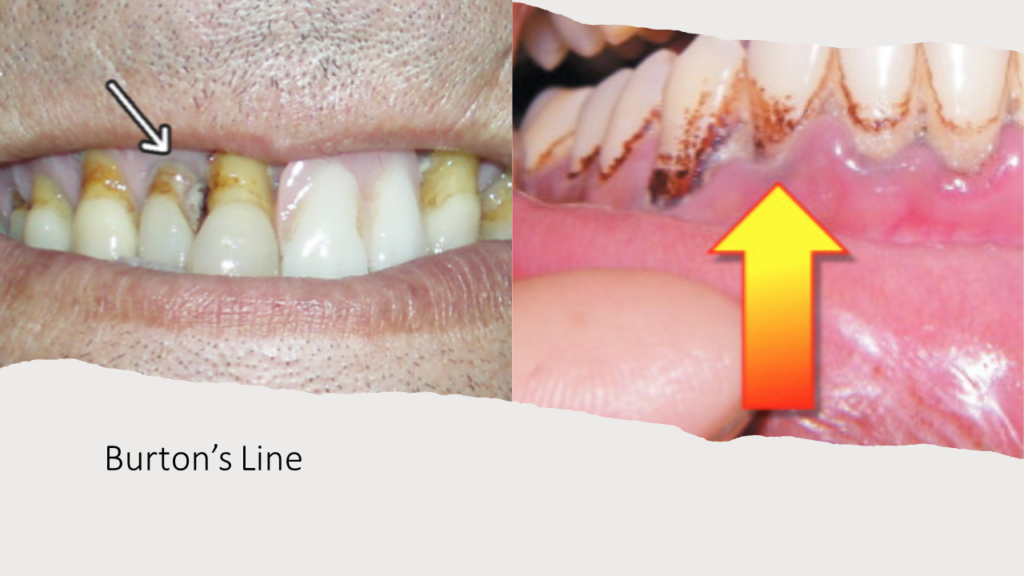
Burton’s line might be an important clue that can help diagnosis of lead poisoning. It is a very thin, black-blue line visible along the margin of the gums, at the base of the teeth in patients with chronic lead poisoning. It is caused by a reaction between circulating lead with sulphur ions released by bacteria in the mouth. This reaction causes deposition of the “black-blue colored” lead sulphide at the junction of the teeth and gums. This clinical sign was first described in 1840 by Henry Burton. However, it’s not a sign reliably present in all patients. But, when present, Burton’s line can be important for clinicians to suspect lead poisoning.
Why is lead considered so poisonous to us?
How does lead cause damage?
Oxygen is life for us. One must imagine oxygen as the “fuel” for life to continue. We need oxygen to generate energy. But the same oxygen that fuels the fire of life also has the ability to burn cells and cause damage. Each time any cell utilizes oxygen, it leads to formation of highly damaging set of molecules known as reactive oxygen species (ROS). ROS is the unwanted residual fire that must been extinguished to protect cellular components from getting damaged.
ROS molecules are extremely dangerous. Damage to DNA by ROS is the most important reason why cancer happens. It is the accumulating damage from ROS that causes ageing. The whole gamut of chronic diseases such as diabetes, hypertension, rheumatoid arthtritis etc end up destroying organs only because of excessive release of ROS for a long period of time.
More the release of ROS, more will be the damage. Faster the release of ROS, faster will be damage. And if the quantity and rate of ROS formation crosses body limits, the damage done is usually permanent.
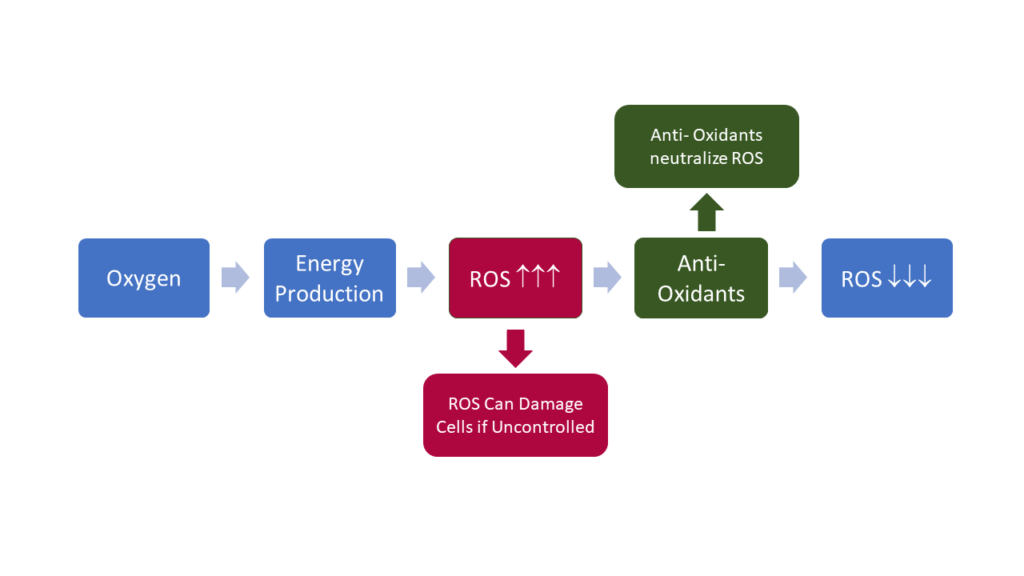
The unavoidable unlucky part is, ROS is produced each and every second in every cell in ay living body. Luckily all our cells are equipped with a set of chemicals known as antioxidants which act as “fire- extinguishers”. These antioxidants neutralize any ROS that is being formed due to utilization of oxygen. So long as ROS is completely neutralized, little damage will happen. And even that little damage will get completely taken care of by our body’s repair systems. However, as we grow older our capacity to produce antioxidants keep diminishing and our repair systems also keep getting weaker. This leads to small amount of cellular damage accumulating on a continuous basis- the extent of damage increasing with time and not getting repaired. We call this process as aging.
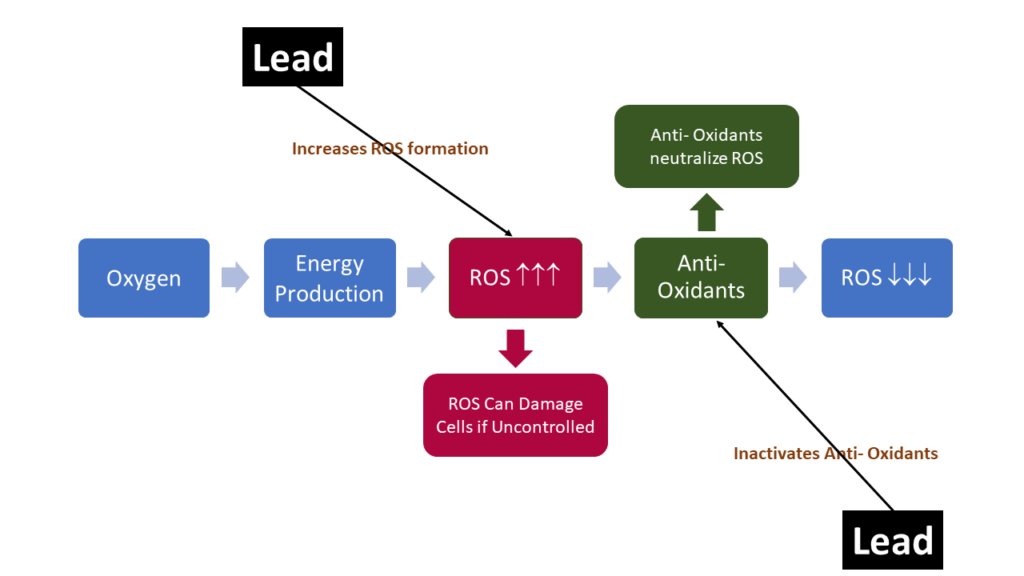
Lead, when introduced in human body, immediately starts producing reactive oxygen species (ROS) molecules such as hydro peroxides, singlet oxygen, and hydrogen peroxide. In ideal scenario, these ROS molecules would be deactivated by the cellular antioxidants. But that depends on how much ROS is produced, since we don’t have unlimited reserves of antioxidants.
And now what if I say lead deactivates antioxidants as well?
Lead has a unique chemistry with 82 electrons of which 4 are valence electrons. If you are naïve to chemistry, its ok. What you just need to understand is that lead loves to combine with Sulphur. Lead also easily interacts with zinc. Sulphur is a very important component of our cellular antioxidants. Similarly for antioxidants to work, zinc is needed. So, when a small amount of lead enters our body it starts combining with all the sulphur present within the antioxidants in each cell. Similarly this lead also goes on to replace the zinc ions which are needed to activate antioxidant system.
The result is devastating. Antioxidants get paralyzed. The “fire- extinguishers” are no longer functioning. Lead itself produces high amounts of ROS. And with no antioxidants to counter, these ROS molecules go unchecked and create havoc. The extent and pace of devastation depends of how fact and what amount of lead has gone in.
Lead poisoning leads to production of reactive oxygen species (ROS) and deactivation of anti- oxidants. The unrestricted damage caused by ROS is the main mechanism of lead poisoning.
Studies conducted in past 20 years have confirmed that lead is poisonous and has lethal effect on the general population. The Second NHANES study conducted in 4292 individuals in 1976-1980 evaluated health care outcomes for various lead levels in blood. These individuals were followed up until 1992.This study showed that individuals with blood lead levels of 20–29 μg/dl (15% of the U.S. population at that time) had 46% higher deaths (due to any cause), 39% higher deaths due to heart diseases and 68% higher deaths due to cancer. The Third NHANES study that was conducted during 1988–1994 in 13,496 individuals showed that lead is hazardous for heart even when blood lead is < 10 μg/ dl.
Toxic effect of Lead on Blood System
Hemoglobin is what makes your blood red. Hemoglobin is present inside red blood cells (RBCs) and is necessary to carry oxygen from lungs to all the cells across the body. Lead poisons the chemicals required for production of hemoglobin in blood. The ROS produced by lead also damages the cell membrane of RBCs. This severely disrupts RBCs’ capacity to carry oxygen. This condition is known as anemia.
As discussed in an earlier section, lead poisoning results into two forms of anemia:
- Frank anemia, is hypochromic and normocytic or microcytic with a reticulocytosis. (for simple explanation of these terminologies look into the earlier section). This form of anemia appears only when there is chronic lead intoxication for a considerable period of time and
- Hemolytic anemia. In this form of anemia RBCs just die off and is related to acute high levels of lead exposure.
We also saw that disruption of hemoglobin synthesis leads to accumulation of ALA in blood. This ALA can be detected in urine even at BLL of <10 μg/dl. ALAD inhibition by lead occurs at BLL of 10–20 μg/dl. However, body is able to produce enough hemoglobin until BLL reaches about 55 μg/dl. This just means that anemia would be seen only when lead is more than 5 times higher than the acceptable levels. Hence urine ALA is used for early diagnosis of lead poisoning.
Toxic effect of Lead on the Neurological System
Brain is highly sensitive to lead poisoning and gets easily damaged. Neurons are the critical cells that form our brain and neurological system.

Accumulation of porphyrins and ALA from disrupted hemoglobin formation is toxic to these neurons. Lead also blocks functioning of essential components of our neurological system such as neurotransmitters and ion channels. For brain to function and for nerves to transmit signals cations such as Ca2+, Mg2+, Fe2+, Na+ are essential. Lead interacts with these cations and destroys the channels necessary for signal transmission.
Every system in our body is so well planned that it is nothing less than a miracle in action. Because brain is such a critical organ for us, there are well developed systems to protect it. To protect from external damage brain is located inside the tough body cage called cranium (we call it skull). Inside cranium there are membranes and fluid filled cushions that act as shock absorbers and provide additional protection to brain. However, toxins and germs can enter blood via food or air and through blood these toxins can reach brain.
But it’s not that easy for any toxin or a germ in blood to simply enter brain. Blood entering brain has to through a protective filter mechanism that effectively stops any such toxin or germ in blood from entering brain. This protective filter mechanism around brain is known as blood brain barrier (BBB). However, critical components necessary for brain functioning such glucose, oxygen, nutrients etc are allowed by BBB to enter to brain from blood. The amount allowed to enter is also controlled by BBB and depends on brain’s requirement for that nutrient.
One such critical component that is allowed by BBB to enter brain in a controlled fashion is calcium. And this is where BBB fails to prevent lead from entering brain. When blood contains toxic levels of lead, lead simply replaces calcium ions with itself.
BBB gets fooled and its mistakes lead for calcium. Thus, when brain asks for calcium, instead of calcium, lead goes in.
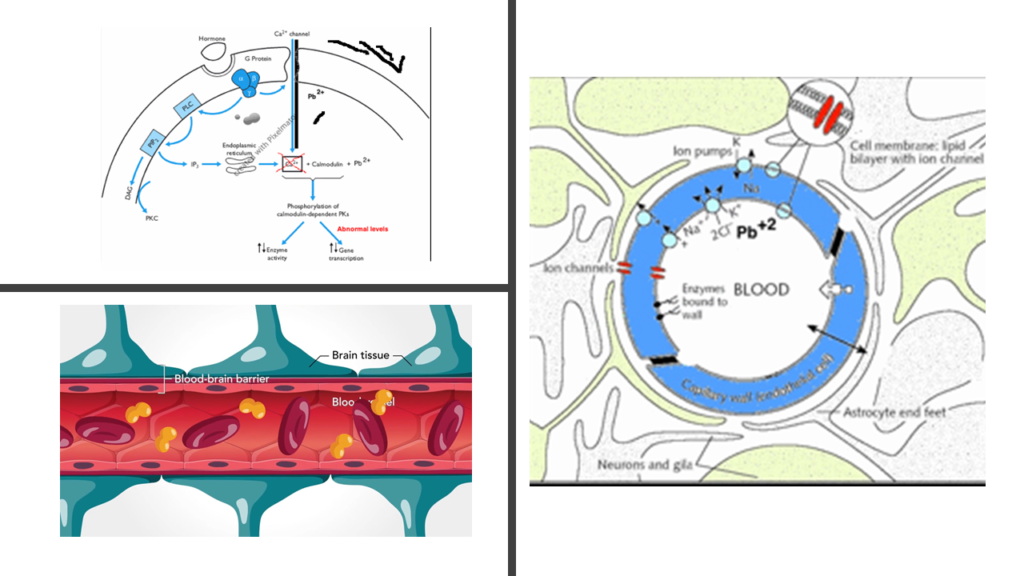
Nerves connect brain to rest of the body- signals from brain get transmitted via nerves. In adults, both nerves and the brain are equally affected. In children, since brain is rapidly developing, the damage to brain is instantly visible and is more pronounced. By poisoning key brain systems (viz. N-methyl-D-aspartate receptors and Protein kinase C– you need not remember these names!) memory formation and thought generation processes are significantly impacted.
Brain fails to effectively generate any signals that are used to control other parts of the body. Because the nerves are also damaged by lead, whatever little signals are sent by brain are also not efficiently transmitted by these damaged nerves. This results in issues with muscular coordination, fatigue and muscular weakness.
Many studies have proven that even very low BLL may impact children’s cognitive abilities and lead to learning deficits, lowered intelligence quotient (IQ) and behavioural problem. The problematic finding is that reduced academic performance is associated with BLL lower than 5 μg/dl.
A recent study published in Proceedings of the National Academy of Sciences (PNAS) past century of lead exposure lowered IQ Score of half of Americans, leading to a loss estimated of 824 million IQ points since the 1940s
This just means that there is no lower level of lead in blood which can be regarded as safe. Ignore if CDC said 5 μg/dl is the lower limit. Lead simply should not be present in blood.
Researchers now argue that argued that for every 10 μg/dl increase in blood lead, there is a loss of 4–7 IQ points. At low level of lead exposure children might be hyperactive, easily irritated and non-attentive. As the lead levels go higher, they start witnessing decreased intelligence, delayed growth, hearing loss and issues with memory. Soon high lead levels will result in permanent brain damage and death. Exposure to lead during prenatal period (when baby is inside mother’s womb) and early childhood has been shown to be associated with violent crimes in adulthood.
Acute encephalopathy is a dangerous outcome that can occur in children at BLL of 80–100 μg/dl and in adults at BLL of 100–120 μg/dl. A patient with acute encephalopathy suffers from irritability, agitation, headaches, confusion, ataxia, drowsiness, convulsions and coma. Studies in in lead workers with BLL > 40 μg/100 ml reveal neurobehavioural effects including disturbances in reaction time, visual motor performance, hand dexterity, IQ, cognitive performance, anxiety and mood.
Toxic effect of Lead on Bones
In our body lead gets stored primarily in our bones. Lead that gets deposited in the deeper parts of bones remain confined to the bones. However, the deposition on the bone surface remains accessible for mobilization into blood.
Sustained exposure of lead for years, leads to prolonged buildup of lead in bones which is re-absorbed into blood over a long period of time. Lead mobilization from bones into blood depends upon number of factors such as extent and period of exposure to lead, age, pregnancy etc. In case of pregnant women and children whose bones are in a developing stage, there is a constant remodeling of bones. This remodeling leads to constant sustained release of stored lead especially on the surface of bones, into the blood stream.
Toxic effect of Lead on Reproductive System
In women, lead toxicity leads to infertility. If exposed to lead during pregnancy it can lead to complications such as premature delivery, pregnancy hypertension, miscarriage etc. Increased BLL can delay puberty in girls. Lead directly impacts functioning of a compound called human chorionic gonadotropin (HCG) which is critical for any successful pregnancy. Research has shown that the risk of spontaneous abortion doubled at BLL of 5–9 μg/dl. As we saw earlier, bones store the highest content of lead. Metabolic changes during pregnancy mobilizes the lead from bones into the blood thus increasing the toxic effects of lead. Lead impacts severely the baby that is growing in the womb of a mother exposed to lead. Pre-natal exposure to maternal BLL of 14 μg/dl may be subjected to increase the possibility of reduced birth weight and premature birth. Such pre-natal exposure may be related with an increased hazard of developmental abnormalities. Scientists have observed higher amount of learning disabilities among school children whose parents were lead-poisoned when they were children 50 years back
As in females, lead poisoning leads to infertility in males as well. At BLL > 40 μg/dl lead damages the sperms, disrupts functioning of testosterone (the male hormone) and decreases libido. More the BLL more is the damage of sperms, as has been observed in workers from battery manufacturing factories.
Toxic effect of Lead on Kidneys
Environmental exposure to lead even at low levels (~10 μg/dl) damages the kidneys. Kidneys are the filters of our body that remove all the unwanted wastes from our blood. This filter consists of the main filtration organ known as glomerulus and tubes that carry waste as urine. These tubes are known as renal tubules. The tubules ensure that nothing important gets thrown out into urine. Damage to renal tubules by lead leads to glucose and proteins getting removed into urine (leading to glycosuria and aminioaciduria). There are two types of kidney damage (known as nephropathies) caused by lead toxicity: acute (due to sudden exposure to large amount of lead) and chronic (due to long term exposure). In acute lead induced nephropathy, the internal lining of the renal tubules get eroded. This causes secretion of proteins into urine. Similarly, phosphates and glucose also start appearing in urine. This condition is also known as Fanconi’s syndrome. It also needs to be mentioned here that lead toxicity itself causes increased breakdown of body tissues that increases the amount of phosphates, glucose and proteins in blood, that finally reaches the kidneys. In chronic nephropathy slowly glomerulus and tubules suffer irreversible damage. This leads to hyperuricemia (increased uric acid in blood), hypertension and kidney failure. And all these damages happen due to the excess ROS generated by lead and disruption of the antioxidants.
At initial stages this kidney damage can be reversed if accurate treatment starts. Hence early diagnosis of lead poisoning is so important.
Toxic effect of Lead on Cardiovascular System
In a large study conducted between 2001 and 2002 (Baltimore Longitudinal Memory community study) researchers found that higher lead levels caused hypertension. Lead poisoning damages the heart and blood vessels that carry blood from heart to all the other organs. Damage to the blood vessels make them lose their elasticity. The also start becoming narrower. This leads to increase in blood pressure (this is known as hypertension). ROS unleashes its damaging impact on heart increases the chances of complications such as heart attacks.
Lead Can Cause Cancer
The International Agency for Research on Cancer (IARC) has defined which chemicals can cause cancer. Such cancer causing chemicals are known as carcinogens. As per IARC classification, chemicals falling under Group 1 and Group 2 can cause cancer. Group 3 chemicals are those which might be carcinogenic, but sufficient evidence is still awaited. Inorganic lead compounds fall in Group 2A carcinogens as they are expected to cause cancer while tetraethyl lead (organic lead) may also cause cancer, but is a Group 3 carcinogen. The National Toxicity Programme, USA has already suggested that lead can cause cancer. Same is the view of the US Environmental Protection Agency as per its 2011 report. There are amble evidences from laboratory and animal studies that prove lead is a carcinogen. Lead acetate causes kidney cancer in animals. Similar data is emerging from human studies as well. In one study organic lead was identified as a carcinogen that led to rectal cancers in factory workers. Some studies have shown lead causing stomach cancer and lung cancer in humans.
| Group | Description | Definition |
| Group 1 | Carcinogenic to humans | Sufficient evidence of carcinogenicity OR Evidence of carcinogenicity in humans is less than sufficient but there is sufficient evidence of carcinogenicity in experimental animals and strong evidence in exposed humans that the agent acts through a relevant mechanism of carcinogenicity |
| Group 2A | Probably carcinogenic to humans* | Limited evidence of carcinogenicity in humans and sufficient evidence of carcinogenicity in experimental animals OR Inadequate evidence of carcinogenicity in humans and sufficient evidence of carcinogenicity in experimental animals and strong evidence that the carcinogenesis is mediated by a mechanism that also operates in humans OR Limited evidence of carcinogenicity in humans, but belongs, based on mechanistic considerations, to a class of agents for which one or more members have been classified in Group 1 or Group 2A |
| Group 2B | Possibly carcinogenic to humans* | Limited evidence of carcinogenicity in humans and less than sufficient evidence of carcinogenicity in experimental animals OR Inadequate evidence of carcinogenicity in humans but sufficient evidence of carcinogenicity in experimental animals OR Inadequate evidence of carcinogenicity in humans and less than sufficient evidence of carcinogenicity in experimental animals, but with supporting evidence from mechanistic and other relevant data |
| Group 3 | Not classifiable as to its carcinogenicity to humans | Evidence of carcinogenicity is inadequate in humans and inadequate or limited in experimental animals OR Evidence of carcinogenicity is inadequate in humans but sufficient in experimental animals, but strong evidence that the mechanism of carcinogenicity in experimental animals does not operate in humans OR Agents that do not fall into any other group Agents in Group 3 are not determined to be non-carcinogenic or safe overall, but often means that further research is needed. |
| Group 4 | Probably not carcinogenic to humans | Evidence suggesting lack of carcinogenicity in humans and in experimental animals OR Inadequate evidence of carcinogenicity in humans but evidence suggesting lack of carcinogenicity in experimental animals, consistently and strongly supported by a broad range of mechanistic and other relevant data |
Scenario of Lead Exposure in India

Dr T V Venkatesh is known as the ‘The Lead Man of India’. Dr Venkatesh, a professor at St. Jones National Academy of Health Sciences conducted a very important study in 1997. In this study, conducted across the seven metro cities in India, BLL of 23,000 children under 12 yrs of age was investigated. 51.3% of these children had BLL >10 μg/dl. At this level there is severe negative impact of the IQ of children. This study marked the beginning of involvement of state in fight against lead poisoning. Based on the finding of this study unleaded gasoline was introduced in India in 2000 that lead to reduction of lead poisoning in India.
In 2003 The National Referral Centre for Lead Poisoning in India (NRCLPI) was established in Bangalore in 2003. Its aim is to create awareness amongst the general public and to conduct research on this preventable environmental hazard. School teachers play a very important in shaping lives of children they team. NRCLPI with the support of Quality Council of India initiated mass sensitization programs to educate school teachers regarding lead poisoning. Few such initiatives targeting students and teachers led by NRCLPI and Quality Council of India are:
- Lead Awareness Programme (LAP) for the general public.
- Lead Educator Programme (LEADer) for school teachers.
- Short term undergraduate student research projects to kindle the scientific tempo in the student community.
One of the serious sources of lead poisoning through water as use of sub-standard PVC pipe used for plumbing and irrigation. The Bureau of Indian Standards has laid down quality standards for these PVC pipes to minimize lead contamination. But, unfortunately, there is no law that enforces these standards. Manufacturing of sub-standard products is cheap and such products easily find their way into the market. Rampant use of such sub- standard PVC pipes due to ignorance and easy availability has resulted in striking amount of contamination of drinking water with lead in many Indian cities including Delhi, Kolkata, Kochi, Mumbai, Pune, Nagpur, Nashik and Guwahati. In 2013 Times of India published a news article regarding a study conducted by doctors in Kolkata. As per this article the study indicated at least 20% of Kolkata city’s children had alarmingly high levels of lead.
India is an epicenter of religion and festivals. Nearly every Hindu house will have one or more idols of gods. Nearly every day is a festival for some community or the other. Leaded paints are rampantly used to decorating idols and are important sources of lead exposure for a large population.
Mass sensitization programs by NRCLPI has been fairly impactful in raising awareness amongst general public. Government bodies, on the advice of NRCLPI, have started notifying about the health hazards of leaded paints.Eeco-friendly cultural festivities are now slowly picking up. The idols for celebrating Durga Puja or Ganesh Chaturthi are now either being decorated with unleaded paints. In many places unpainted water soluble eco-friendly material is used. In 2016 Govt. of India introduced “Regulation of Lead Contents in Household and Decorative Paints Rules, 2016”. Based on this relation, on November 1, 2016 Ministry of Environment, Forest and Climate Change notified that the permissible lead content in the household paints should not exceed 90 ppm.
Such proactive steps from Indian government towards prevention of lead poisoning led the to the 2015 Maggi controversy. In this high profile case, in 2015, some samples of Nestle’s Maggi noodles were found to have lead at levels that were almost 17 times higher than permissible limits. Based on this finding, the Food Safety and Standards Authority of India (FSSAI) conducted a nationwide investigation in which Maggi samples from all across India was collected and tested. Through these tests FSSAI confirmed presence of alarmingly high lead content. Based on this finding, Government on India and Supreme Court issued nationwide ban of the Maggi noodles. Nestle had to withdraw and destroy Maggi worth 320 crores. For 5 months no Maggi was available in any store in India. Nestle had to revisit its production and supply chain processes to ensure Maggi noodles are safe. Only after clearance through lab tests conducted under the supervision of Supreme Court finally Nestle could reintroduce Maggi noodles in the Indian market.

Treatment of Lead Poisoning
Treatment Strategy
The first and most critical step prior to the treatment is the removal of patient from the site of exposure. This should be followed by identification and elimination of possible sources of lead. The Advisory Committee on Childhood Lead Poisoning Prevention (ACCLPP) is a part of CDC, USA. ACCLPP has defined a detailed action plan to combat lead poisoning. While any BLL >5 μg/dl is always a cause of concern and needs intervention, BLL >70 μg/dl is considered as critical and needs immediate hospitalization followed by rapid chelation.
Chelation therapy
Chelation therapy uses certain compounds called chelating agents. These chelating agents bind “toxic” lead ions to form “non-toxic” complex structures called ‘chelates’. They specifically remove the lead from desired site resulting in reduction of body lead burden. Chelation therapy is very useful in treating acute lead poisoning and can save lives. But just one cycle of chelation therapy might not be enough though. In most cases lead levels in blood rebound in patients after chelation therapy and repeated courses become mandatory.
| Sr. No. | Chelating agent | Indication |
| 1 | Dimercaprol | BLL ≥ 70 μg/dl (Combine with CaNa2EDTA if BLL > 100 μg/dl) |
| 2 | CaNa2EDTA ( Calcium Disodium Edetate ) | BLL ≥ 45 μg/dl or in case of lead encephalopathy |
| 3 | D-penicillamine | BLL 45–69 μg/dl; Not recommended for children <6 months |
| 4 | DMSA (Di-Mercapto-Succinic-Acid) | BLL 45–69 μg/dl; Not recommended for children <12 months |

Alternate Therapies
As already discussed at length, the main mechanism by which lead imparts its toxic effects is through unchecked formation of ROS. The main focus of these alternative therapies besides removing lead from the body is to counter this ROS formation. While I elaborate these alternate therapies, I must make it very clear that more evidences are needed in order to advocate safety and efficacy of these alternate therapies.
Garlic seems to be significantly effective in reducing BLL in patients with chronic lead poisoning.
In a well designed study on 117 battery plant workers one group was given 400 mg of dried powdered garlic or 2 g fresh garlic given 3 times a day for 4 weeks. Other group was treated with D-penicillamine (250 mg/3 times daily). Garlic therapy effectively reduced neurological effects of lead poisoning such as irritability and headache. Rate adverse effects was significantly lesser in the garlic group compared to those on treatment with D-penicillamine.
Coriander is also believed to be extremely effective in lead poisoning.
Experts believe that coriander accelerates filtering out of lead from blood into urine. Treatment with coriander was studied on children having high BLL (163.81 ± 57.19 μg/L). In these children it was observed that coriander significantly decreased BLL.
Thiamine, Vitamin B1, (25–50 mg/kg/day) along with CaNa2EDTA (50 mg/kg/day) for 3 days reduces the damage caused by ROS in addition. This combination also accelerates elimination of lead from liver and kidney.
Vitamins C and E are also believed to counter ROS induced damage in lead poisoning.
N-acetylcysteine (NAC) (800 mg/kg/day) for 5 weeks not only acts as lead chelator but is also an antioxidant that shields against ROS. One must note that NAC is widely used to treat paracetamol poisoning and there NAC effectively counters ROS. Studies suggest that maybe N-acetylcysteineamide is a better alternative to NAC as it has a better ability to bind to lead and has cellular permeability and systemic bioavailability than NAC.
Taurine 50-100 mg/kg once daily with DMSA (Di-Mercapto-Succinic-Acid) 50 mg/kg once daily for 5 days is effective treatment against sub-chronic lead poisoning to reduce lead burden. However single therapy with Taurine is not able to impart the same effects and needs the chelation effect provided by DMSA.
We have seen that Sulphur is an important component of antioxidants. Sulphur containing compounds such as Alpha-lipoic acid (50 mg/kg/day), methionine (100 mg/kg/day) and homocysteine (25 mg/kg/day) administered for 5 weeks are also able to counter the oxidative stress due to ROS in lead-exposed tissues.
Prevention of Lead Poisoning
Ronald Lane’s pioneering work on lead poisoning as occupational health hazard in 1949 was the start of a movement that focused on effective and formal control of exposure of lead workers. The words from his 1949 paper, published in British Journal of Industrial Medicine, still hold true even after more than 70 years. In this landmark paper Ronald Lane had said that- “There is only one way to prevent lead poisoning and one way only and that is to make the process safe.” The paper also says the following- “The importance of education of the worker himself must be stressed. He must understand fully the dangers of his work. No attempt must be made to hide it or to minimize it but he must, at the same time be shown his own responsibilities in any safety program. This needs patience and hard work on the part of the doctor. Complete success will be impossible without the co-operation of the workman.“
Even today the the best way to prevent lead poisoning is avoiding exposure to lead. Lead poisoning is completely preventable. Such prevention is crucial because the lead exposure induced brain damage amongst young children is irreversible. Frequent hand washing must be emphasized and children must be discouraged from putting their hands in the mouth. In case of old buildings, children should constantly be kept under strict vigil and must be discouraged from ingesting the paint “chips” chipping off the walls. Frequent vacuuming can help. And so would eliminating the use of lead containing objects like artificial jewelry etc. Sub- standard house pipes containing lead can easily contaminate drinking water and must be replaced. Ban on usage of leaded gasoline and paints has been very successful in lowering the BLL in the US. In factories strict adherence to industry safety regulations is necessary to regulate and control occupational lead exposure. Workers and family members must be constantly educated to prevent lead poisoning from being carried from factories to homes.
Adequate nutrition can help mitigating impact of lead exposure. Zinc deficiency is known to worsen lead poisoning. Deficiency of zinc, vitamin C, protein or phosphorus increase the absorption of ingested lead from stomach into blood. Iron deficiency is associated with elevated BLL. Hence it is recommended to put children with lead poisoning on iron rich diet. Some studies have even suggested that iron supplementation itself can decrease BLL in children irrespective of iron deficiency. Calcium also decreases lead absorption. Thus, these nutritional deficiencies must be addressed to ensure a successful fight against the menace of lead toxicity. Today there are genetic tests available that can help identify an individual’s sensitivity to lead poisoning- some people are more prone than others to suffer from lead poisoning at low BLL compared to others. Such tests might be used to for mass screening and protect these susceptible individuals.
Final Comments
Lead poisoning is a serious socio- environmental hazard. Its is highly possible that unknowingly we are exposing ourselves and our children to lead poisoning. PVC pipes carrying water to our homes can easily be the source of such lead poisoning. So can be the innocent looking toys that we lovingly gift our children to play with. From the kajal applied on eyes to the deities that are worshipped in so many houses- all might be the slowly poisoning us with lead.
Although there is some guidance from experts in terms of what can be the maximum level of lead in blood, it is a well-known fact that no level of lead is safe for us. Even at extremely low levels, lead causes brain cells to die. Prevention of lead poisoning is extremely critical as much of the damage caused by lead is irreversible.
Diagnosis of lead poisoning is very difficult- in most of the cases there are literally no symptoms for years. Even if there are symptoms, these are so non-specific that its difficult to suspect lead poisoning based on these symptoms. Hence, even at the slightest suspicion, thorough investigations are needed.
Chelation therapy is the most common treatment. But it has its own drawbacks. In most cases lead levels in blood rebound in patients after chelation therapy and repeated courses become mandatory.
Government has initiated significant steps in educating masses regarding lead poisoning and enacting industrial laws. Still, sub-standard products with significant lead content continue to find their way into our houses across. Silently millions might be suffering from lead poisoning.
Its our moral duty to educate ourselves and everyone about lead poisoning and do our part in curbing this issue. This post is an extremely small attempt from my end. Can you also play your part? What are your thoughts? Please post your view in the comments section.




Very uSeful information. Thanks Dr Roy. So having iron pipe for water supply is better than PVC . We just changed iron pipes with pVC.
Good quality PVC pipes should be ok. Avoid cheap PVC pipes which might bypass government norms regarding lead.
Reading your article helped me a lot and I agree with you. But I still have some doubts, can you clarify for me? I’ll keep an eye out for your answers.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://accounts.binance.com/bg/register?ref=OMM3XK51
Hello. Thank you for always good blog
Hello. Thank you for always good blog
Hello. Thank you for always good blog
Hello. Thank you for always good blog
This is a great tip especially to those fresh tothe blogosphere. Simple but very precise info… Appreciate your sharingthis one. A must read post!
Good information. Lucky me I recently found yourblog by accident (stumbleupon). I’ve book-marked it for later!
Hello. Thank you for always good blog
Hello. Thank you for always good blog
Hello. Thank you for always good blog
Hello. Thank you for always good blog