Human biology varies with seasons and climatic conditions. Just changes in daylight conditions significantly impacts cellular processes. Then, how come we expect same medicine to work to treat a disease similarly in all seasons and climates?
Recently I read a research paper that was published in the journal “Nature Communications”. This paper titled “Widespread seasonal gene expression reveals annual differences in human immunity and physiology” explained findings from a research conducted by scientists from UK and Germany.
As I read the full text, I understood how critically important the findings were from treatment perspective. This is something every doctor should know.
So, in this blog, I will explain findings from this research and how those findings can revolutionize treatment of diseases.
Seasonal changes affect all living things, as shown by seasonal physiology and behaviors in plants and animals. For example, when a foreign skin is transplanted into a lizard, lizards body fights off this transplanted skin with a reaction. But this reaction completely depends on on the season when the skin was grafted. This indicates that graft rejection in reptiles is under the control of seasonal conditions. Studies conducted in squirrel monkeys show strong relationship between seasons and physiological systems. Squirrel monkeys start experiencing increase in body weight and steroid hormone levels during specific months of the year. This physiological shift influences breeding behavior and sexual interactions.
Seasonality of infectious diseases is well known in humans. We speak of ‘flu season’ in winter, without ever wondering why it might be the case although influenza viruses circulate year-round. Entero-viruses typically show late summer or early autumn seasonality, whereas such viruses as rotavirus and noroviruses cause infection in cold, winter months. In the USA, the incidence of echovirus, coxsackie A and coxsackie B viral infections was shown by Moore to be profoundly seasonal, with a peak incidence in August of each year. It has been suggested that a natural physiological rhythm may explain the seasonality of infectious disease diagnoses and their effects.
In humans, many complex diseases that involve multiple genes, such as cardiovascular, autoimmune and psychiatric disorders, have seasonal patterns of occurrence and severity. Some biological processes in humans change with seasons, including ones that play important roles in immunity, such as vitamin D metabolism. The loss of skin color as humans moved out of Africa to cooler and less sunny areas to increase vitamin D production from sunlight is a major example of how humans adapted to different environments over time.
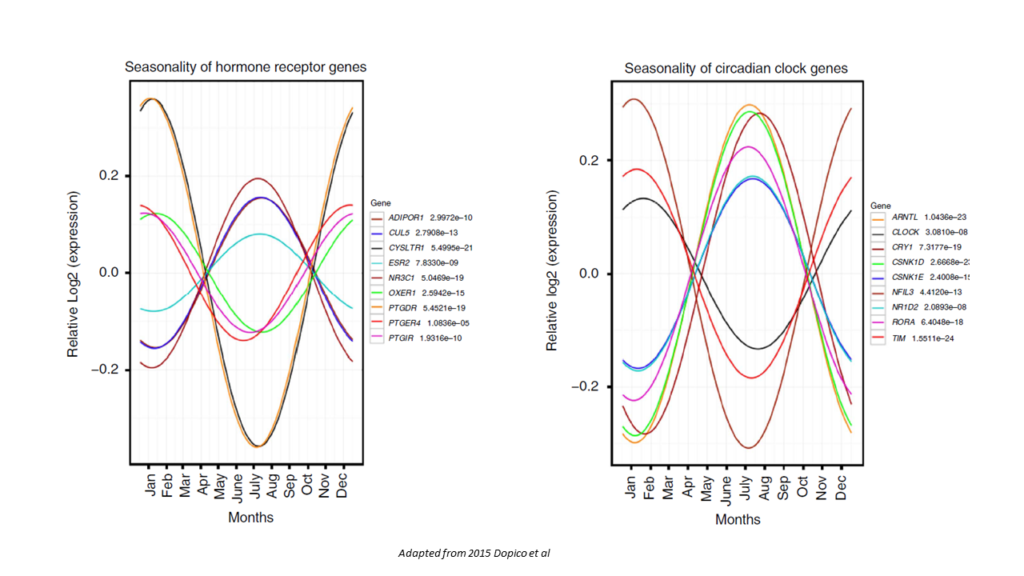
We all know that genes code for whatever is produced in our cells. But, presence of any gene doesn’t mean anything, until it is switched on. Each cell in our body behaves in particular way depending on which genes are switched on at that point in time. This switch depends on conditions that the cell is facing. Wrong gene switched on at wrong situation can be harmful. All cells in our body seem to have some form of molecular clocks that can switch on or switch off expression of one or more genes depending on external season and climatic conditions. One example of such molecular clock is the anti-inflammatory circadian transcription factor called ARNTL (also called BMAL1)- scientists believe that this molecular clock has seasonal differences because daylight sets the circadian rhythms in mammals.
The study that I am discussing in this blog aimed to understand how seasons might affect the molecular details of human physiology. In this study, the researchers explored the seasonal variations in gene expression and cellular composition of blood in humans. The research was conducted by a team of scientists from various fields, including immunology, genetics, and epidemiology. By bringing together experts from different disciplines, the study was able to provide a more comprehensive understanding of how seasonal variations impact human immunity and physiology.
For conducting this research, these scientists analysed mRNA expression levels in peripheral blood mononuclear cells and adipose tissue biopsies, full blood count data, and the circulating levels of inflammatory protein biomarkers. The biological samples represented ethnically and geographically diverse populations.
The study revealed over 4,000 protein-coding mRNAs in white blood cells and adipose tissue that have seasonal expression profiles, with differences observed between Europe and Oceania. Additionally, the cellular composition of blood varies by season, with differences between the United Kingdom and The Gambia.
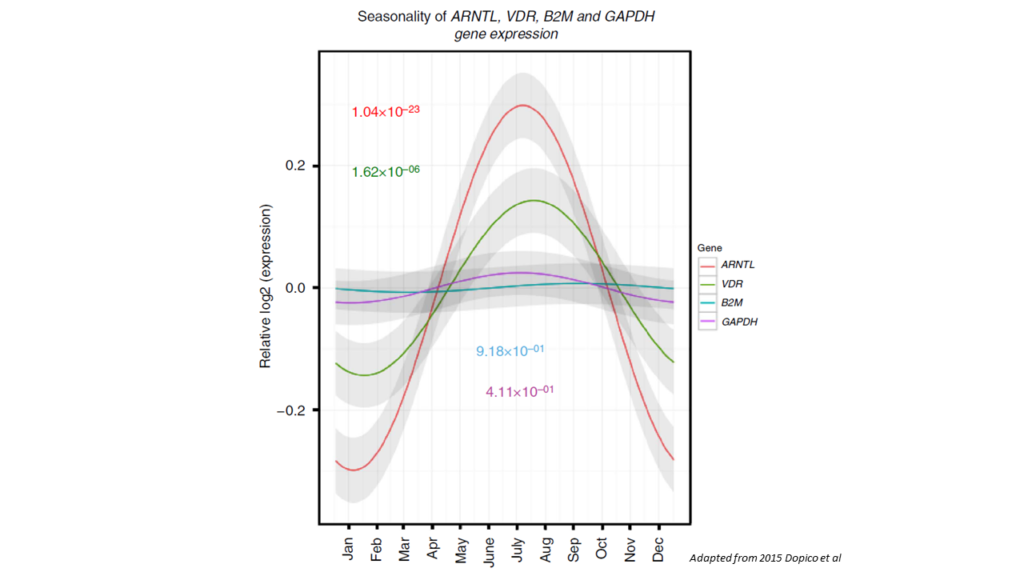
One of the most significant findings of the study was the profound pro-inflammatory transcriptomic profile during European winter. This profile was characterized by increased levels of soluble IL-6 receptor and C-reactive protein, which are risk biomarkers for cardiovascular, psychiatric, and autoimmune diseases that have peak incidences in winter. These findings suggest that there may be a link between seasonal variations in gene expression and disease susceptibility. The study also found that the immune system undergoes significant changes throughout the year. Co-regulated seasonal mRNAs were identified revealing seven winter-expressed modules with more frequent pro-inflammatory processes compared to summer-expressed modules. These findings suggest that immunological function varies seasonally, which could explain some of the observed differences in disease incidence between seasons.
The research has important implications for personalized healthcare approaches that take into account seasonal variations in human physiology. By understanding how gene expression and cellular composition vary throughout the year, healthcare providers can develop more effective treatment plans tailored to individual patients’ needs. For example, patients with autoimmune diseases may benefit from increased monitoring during winter months when pro-inflammatory processes are more frequent. Similarly, patients at risk for cardiovascular disease may benefit from increased monitoring during winter months when risk biomarkers are elevated. The study also highlights the importance of considering environmental factors when developing personalized healthcare approaches. For example, patients living in regions with significant seasonal variations may require different treatment plans than those living in regions with more stable climates.
The study also underscores the importance of considering environmental factors when developing public health policies. By taking into account seasonal variations in disease incidence and risk factors, policymakers can develop more effective strategies for preventing and treating diseases. For example, regions with significant seasonal variations may require different public health policies than regions with more stable climates. In areas where winter is associated with a higher incidence of cardiovascular, psychiatric, and autoimmune diseases, policymakers may need to implement measures to reduce exposure to risk factors during this season.
The study also raises important questions about the underlying mechanisms that drive these seasonal variations. For example, what role do environmental factors such as temperature, humidity, and daylight hours play in regulating gene expression and cellular composition? How do these factors interact with other physiological processes to influence disease susceptibility?
Answering these questions will require further research, but the study provides a valuable starting point for future investigations. By identifying the seasonal variations in gene expression and cellular composition of blood, the study provides a roadmap for future research into the underlying mechanisms that drive these changes.
While modern science is still discovering how seasonal variations impact genomic expressions and how those interactions can guide treatment of diseases, the ancient science of Ayurveda deeply recognizes this aspect of medicine. Ayurveda not only outlines in detail how seasons can impact a disease, it also specifies that each such interaction between climate and individual is unique to that individual. The beauty and depth of Ayurveda lies in the fact it also recognizes how human biology varies throughout the day from morning till night. In Ayurveda each individual gets his/her own unique personalized treatment for the same disease. And for the same individual, for the same disease, treatment strategy may change in Ayurveda depending on several other factors including the season. In Ayurveda, treatment of a disease depends on patient’s unique Prakriti, presenting symptoms, dietary patterns, daily habits and imbalance in the doshas. Ayurveda will not only prescribe a medicine but also will advocate on certain behaviors and dietary regimes. The choice of treatment interventions also varies according to age, mental state, the season (climate and other environmental factors), etc.

To be honest, it is simply hard for me to understand why don’t we study which medicine will be more impactful in which season. Circadian rhythm and seasonal variations in human physiological processes is well established. When human biology varies with season, it is a simple logic to comprehend that same medicine will have variable impact depending on the season and climate. And we, as doctors, will be foolish to ignore this fact.


My relatives all the time say that I am killing my time here at net, except I know I am getting know-how every day by reading thes pleasant articlesor reviews.