I am a medical doctor with specialized training in treating diabetes, and have been quite successfully managing patients. So, this post is quite close to heart and through this post I intend to share a treatment philosophy that, I believe, each doctor must remember while treating any patient with Type 2 Diabetes Mellitus.
I will be explaining all concepts in this post using extremely simplified language and analogies, so that any one without any medical knowledge may benefit. And I have tried my best to maintain scientific validity of everything that I will explain with proper hyperlinked references that you may use to verify.
Please note that this article is not meant to replace/discredit any recommendation from any doctor. If you are not a doctor, please strictly adhere to your what your physician recommends.
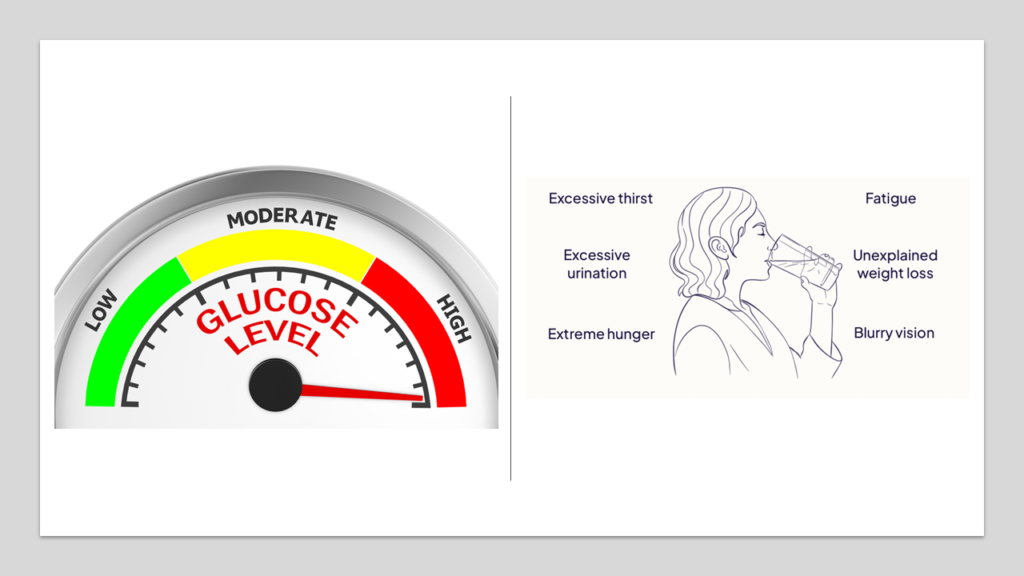
Diabetes is a condition marked by increase in blood sugar. In Type 2 Diabetes Mellitus, this happens because of a phenomenon called insulin resistance. We will soon discuss about insulin resistance in great details. Type 2 Diabetes Mellitus is the most common form of diabetes. It is a disease rapidly afflicting population globally and is now considered a global epidemic.
Sugar is the primary fuel used by our body to generate energy. For this, sugar is absorbed from the food that we eat. When we eat anything, that food reaches our stomach and intestines. Lining these organs is a complex system of blood vessels. The walls of stomach and intestines absorb nutrients including sugar and transfer them into blood. Through the blood, sugar now flows through the entire body, bathing all the cells that would need to generate energy.

But cells don’t allow these sugars to enter just like that.
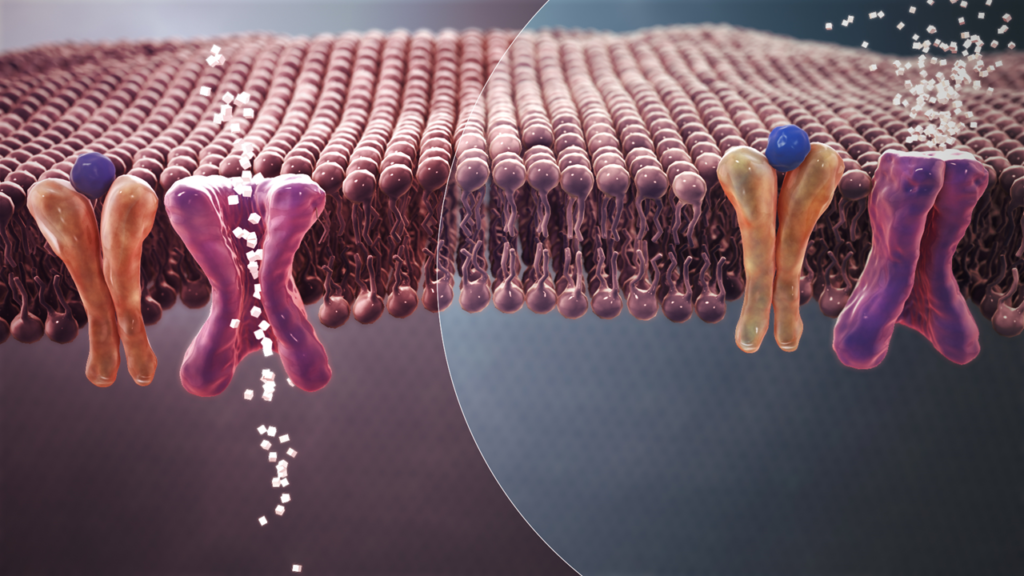
Each cell in our body is like a small office. Cell organelles are like employees. They all work continuously. So, when they are hungry they crave for energy. This energy that keeps the cell going on and on is known as ATP (Adenosine Tri Phosphate). ATP is generated by an engine called mitochondria that is present inside every cell. The primary fuel used for generating ATP is that sugar which is available in the blood. So, only when the cell has to generate energy, it allows sugar from the blood to enter inside it. To facilitate this entry of sugar into the cell, there are doors. Let’s call these doors as sugar doors. These sugar doors are extremely selective– when these doors are opened, through these doors only sugars can come in, and no one else.
And these sugar doors don’t open on their own. These doors can be opened only by highly specialized guards who reside outside the cells. When a cell is hungry, it shouts for sugar. The guards then come and open the sugar doors and let sugar molecules from blood to enter the cell. Upon entering the cell, the sugar molecules are led to a giant engine within the cell called mitochondria. Here, you can imagine sugar as gasoline. Mitochondria then burns these sugar molecules eventually leading to formation of ATP- the energy that runs the cell.
The important part here to note is that sugar doors can be opened only by those specialized guards present in blood. Without the help of these guards, no sugar molecule can enter irrespective of how desperate the cell might be for generating energy.
The role of these guards and the sugar doors completely explains genesis of diabetes. Diabetes happens because guards fail to completely open the sugar doors! These specialized guards are the molecules what we know as INSULIN!

There are two scenarios where this can happen:
Scenario 1: All guards meant to open sugar doors are dead.
Scenario 2: The sugar doors are jammed. In this case, the guards find it difficult to to open the doors completely. The doors are resistant to all the normal efforts made by the guards. The doors have become resistant.
Scenario 1 leads to Type 1 Diabetes Mellitus. This is a rare form of diabetes generally seen in unfortunate children and young adults. It is actually an autoimmune disease where there are antibodies that destroy insulin. In this disease, the primary treatment option is logically to give insulin from outside.(1)
And scenario 2 leads to Type 2 Diabetes Mellitus. The sugar doors are resistant to the opening action of insulin. Insulin is unable to open sugar doors. We call this situation as insulin resistance.(2)
(From here onwards, for the sake of brevity, we will call Type 2 diabetes mellitus simply as diabetes.)
We all dread diabetes. We know it cannot be cured, and once you get this curse you will have to take number of medicines all your life to prevent diabetes from killing you. Diabetes is a leading cause of cardiovascular diseases such as heart attacks and strokes. If uncontrolled, it can destroy almost all organs including eyes, kidneys etc.(3)
And the root cause of diabetes are these sugar doors in our cells that get jammed, thus making it very difficult for sugars to enter inside our cells. Hence the sugar levels in blood start rising. But cells are not able to utilize these sugars. And they are hungry. So, they make you feel hungry. This makes you eat more. A patient with uncontrolled diabetes is always hungry like a beast. But that food doesn’t work since the sugars from the food will just pile up in the blood- they will hardly get any chance to enter cells as the sugar doors are nearly closed. But cells have to work. They can’t just stop functioning. So, when the main fuel (sugar) is not available in required quantities, body cells start burning fats. And this leads to weight loss. A patient with uncontrolled diabetes will experience rapid and significant weight loss. Also, because energy generation is not optimal, such person feels tired and lethargic all day. When fat is primarily used a fuel, it leads to generation some by products known as ketone bodies. They smell like nail polish. A patient with advanced uncontrolled diabetes will have that fruity nail polish like smell in his breath.
Sugar in blood makes it thicker. To maintain normal thickness, your body signals you to drink water more. This makes patient with uncontrolled diabetes always thirsty. High level of sugar in blood is not natural- and kidneys then try to throw this sugar out. And hence, uncontrolled diabetes will make one urinate quite often. And this expelled urine can attract ants since it contains sugar!
Any medical book on diabetes will say Diabetes is characterized by three cardinal symptoms- Polyphagia (increased hunger), polydipsia (increased thirst) and polyuria (increased urination).(4)
Of course, all what I described don’t occur dramatically. Not all sugar doors get shut tightly in all the cells. It’s a gradual process. But these “resistant” sugar doors represent the root cause of Type 2 Diabetes Mellitus. When normal level of insulin cannot open these doors, more insulin is secreted in an attempt to force open these doors. That’s why in patients with Type 2 Diabetes Mellitus, amount of insulin in blood is considerably higher than normal. We call state as hyperinsulinaemia.(5)
So, why do these sugar doors get jammed? And why suddenly this is happening in an epidemic proportion across all geographies?
To answer these questions you have to first understand that our body is like to any machine. Laws of physics apply to every single process that take place in our body. When a machine works, there is always friction which leads to wear and tear. So is true with our body. Anything we do always causes some amount of “friction”. This “friction” manifests in the form of biological fire. We call this biological fire as inflammation. The flame of inflammation is destructive to our cells. Unfortunately, inflammation is inevitable. Each breath we take causes inflammation. Each morsel of food we eat causes inflammation. Even each flow of thought will cause inflammation.
For life to happen and proceed, fire is needed. But the same fire also is the cause of destruction. It’s like running a car. If you start a car, there will be friction within it’s components and this will cause damage. That’s why each car would need regular maintenance. The more the car runs, more will be the requirement of maintenance. The faster the car runs, more frequent will be the requirement of maintenance. And one day, despite all maintenances, the car will eventually die.
Our body is just like this car. Each small activity that happens in our body leads to damage via inflammation. Fortunately, unlike car, our body has in-built repair mechanisms. These in- built repair mechanism are amazing. They control the amount of inflammation generated. They also repair the damages caused by inflammation. As long as all such damages are completely repaired, there is no issue.
When we are young our body has an amazing capacity to limit inflammation. All damages caused by inflammation get repaired completely when we are young. But, as we age, our body’s ability to control inflammation starts dwindling. This means slowly but surely, with age, inflammation keeps rising and increasingly causes more damage. With age, our ability to repair damages also keeps getting weaker. Some amount of damages done by inflammation keep remaining unrepaired. These unrepaired residual damages themselves trigger more inflammation and lead to more damage. Re-inflammation leads to more damages which further cause more inflammation. It’s a vicious cycle the eventually leads to complete destruction.
That’s how we move closer to death as we age.

Now, let’s go back to our mitochondria. This is the engine which uses sugar as gasoline to generate energy. Even here, each act of energy generation leads to inflammation and damage to mitochondria and other components of the cell. When we are young, these damages get easily repaired. But, as we grow older, some damages start remaining unrepaired. Remember, residual damages themselves trigger more inflammation. At some point, the extent of residual damages is so huge that energy generation from sugar is unsustainable. At this stage, any use of sugar for energy generation by mitochondria will lead to unacceptable level of inflammation. And hence, the only way out is to limit using sugar. At this point, cell starts blocking all its sugar doors, although all its employees are shouting with hunger. The guards (insulin molecules) outside the sugar doors try opening these doors. But now it is increasingly difficult for these guards to open the doors. Cell has blocked the doors from inside. This is what we call as insulin resistance.
Insulin is generated in an organ called pancreas. The beta cells inside pancreas are the makers of insulin. When insulin is not able to open the sugar doors, beta cells try to force open the doors by secreting more insulin. That’s why, generally in patients with Type 2 Diabetes mellitus have very high levels of insulin in blood. Initially, high levels of insulin succeed in opening few of the sugar doors. But cells respond by closing the doors even tighter.
In the meanwhile, cells prepare themselves to satisfy energy needs without using sugar. Mitochondria switches to alternative source of energy. And this alternative source is fat. The machinery to derive energy out of fat is still intact and healthy since it has been hardly used. And this leads to weight loss in patients with Type 2 Diabetes Mellitus, as we discussed earlier as well.
The thing we must note here and highlight is that insulin resistance is a desperate defense mechanism to protect the cell form unstainable levels of inflammation that will arise if sugar is used as energy source. Diabetes is a consequence of this decision by the cells to stop using sugar. Closing the doors and not allowing sugars to enter leads to rising sugar levels in blood. It is true that eventually these excessive sugars in blood will cause havoc in all organs. But that’s for later. The immediate unsustainable damage that could have resulted by allowing sugar to enter the cells, gets averted by insulin resistance. Insulin resistance allows our body to dampen and delay the deleterious consequences of inflammation.(6)
What we discussed above now easily explains why the chance of developing diabetes keeps rising as we grow older- why diabetes is more common in elderly. As we age, level of inflammation and residual damages just keep rising until a point comes where our cells start defending themselves via insulin resistance.
And nowadays, more and more younger people are also getting diabetes. But, this just indicates that we are aging faster. Biological age and chronological age are two different things- When we talk about age, we generally refer to chronological age. But, biological age is what determines health and not chronological age. Chronological age is the amount of time a body has spent living after birth. Biological age refers to the condition of the body in terms of its efficiency. A super healthy 80-year-old man can have a body condition matching that of a 50-year-old. Here the biological age of this fit 80-year-old man is then around 50 years. Similarly, a 30-year-old person can have a very unhealthy body with lots of diseases. The body condition of such a person might match that of a 70-year-old person. Here the biological age of this unhealthy 30-year-old man is then around 70 years.
We, as a population, are living in increasingly more “pro-inflammation” lives. We sleep less, we stress more, we eat more. More the level of inflammation, faster will be the aging process. Diabetes can be seen as a result of this aging process. Diabetes is inevitable. It’s like graying of hair as we grow older. It’s just that today we diagnose diabetes more that we could couple of decades back, which make us feel that we are experiencing an epidemic. And of course, since we are aging faster, diabetes is becoming more prevalent.
Now that we know the root cause of diabetes, let me come to title of this article. All the doctors out there- beware of using insulin for treating diabetes!

By taking insulin injections you are trying to force open the sugar doors closed by the cells. If you have read the above explanations, you will agree that in diabetes insulin resistance develops to protect body from far greater damage that can happen if sugar is allowed to enter the cells. Insulin resistance is your friend. The currently popular belief is that insulin resistance is bad. And that is true. But you have to understand the context here. Insulin resistance is a signal that something is wrong. But insulin resistance the protection against that underlying pathology. By using insulin injections, you are breaking this protection. Insulin injections serve as hammer against this protective shield offered by insulin resistance.(6)
In diabetes, cells just don’t want sugar to enter- it’s too damaging. The more insulin you push, the more stronger will be the response from cells to stop insulin from opening sugar doors. Insulin resistance will simply keep growing. One direct measure of insulin resistance is obesity. Obesity is a consequence of insulin resistance, in our body’s attempt to keep down inflammation. Anything that increases inflammation will make body gain weight.
So remember, any attempt to force the cells open up the sugar doors will generate high amounts of inflammation. No wonder, insulin injections lead to significant weight gain.(7)
It has been well established across scientific communities that high insulin can lead to development of cancer.(8–10) This association of high insulin with cancer holds true in both obese and normal-weight individuals, regardless of diabetes, visceral adiposity, or metabolic syndrome status.(11) This observation directly agrees with animal studies showing how insulin injections can promote cancer growth.(12)
In 2013 a study published by Lei Wang’s group showed that use of insulin in patients with diabetes significantly increases the chances of developing colorectal cancer.(13) A similar risk for colorectal cancer with insulin therapy was also reported later in the 2014 study that was published in British Journal of Clinical Pharmacology.(14)
Looking at the various studies on cancer, it really seems our cells do know what is good for them! They really know that when inflammation is high, switching from glucose to fat as fuel is a better strategy. Research is pretty clear- when inflammation is high, low carbohydrate diets have protective effects. Low carbohydrate diets have shown to inhibit cancer formation and increases efficacy of ant-cancer drugs.(15, 16)
In pregnancies, treating diabetes using insulin increases the chances of life- threatening complications like pre-eclampsia. In such cases, those drugs that don’t increase level of insulin have better clinical results for treating diabetes.(17)
Majority of large observational studies show strong dose-dependent associations for injected insulin with increased cardiovascular diseases risk and worsened mortality. It has been duly noted by researchers that over-insulinization with use of injected insulin predisposes to inflammation, atherosclerosis, hypertension, dyslipidemia, heart failure, and arrhythmias.(18)

All these dangers that we discussed above are true not only just for insulin. These dangers are also true for any anti-diabetic drug that works by increasing insulin levels. For example Sulphonylureas are very popular group of anti-diabetic drugs used by doctors across the world. These drugs work by stimulating beta cells in pancreas to create and release more insulin. And hence, these drugs carry the same problems that I noted for insulin. Similar to insulin, they increase the risk of cardiovascular disease and cause weight gain. Plus, they have other challenges as well, which I don’t think I would be able to discuss in this post.(19)
Does this mean we should never use insulin and suphonylureas? No. They have their own places in treating diabetes. Remember, high levels of sugar circulating in blood is will also eventually have devastating consequences. So, if the blood sugar is extremely high insulin injections and sulphonylureas are simply amazing in quickly bringing down blood sugar to manageable levels. Once you have succeeded to bring down blood sugar to such manageable levels, insulin or sulphonylureas should be stopped and patient must be shifted to other anti-diabetic drugs.
Here, one may ask- what are these manageable levels? This question leads to another topic for debate where I don’t agree with how these levels are defined. To me, rising blood sugar is a sign of aging. It’s like graying of hair. It is not liked by anyone. But it is inevitable. High blood sugar, under manageable levels, actually might not do as much harm as we fear. Issue is, these “manageable levels” will vary from person to another. It’s highly inappropriate to use data from population statistics to define health of a single patient. While a fasting blood sugar of 180 mg/dl might be absolutely ok for a 60 year old patient, 150 mg/dl might be too much for another 40 year old patient. Each patient is unique. And here is where it’s the experience and judgement of a physician that matters. Nowadays, by blindly following definitions, we are simply over- diagnosing and over- treating. As I said- this is matter of great debate and I will have to write another long post to explain why I believe what I just explained.

Let me pull myself back to the main topic. As I saying, insulin injections and sulphonylureas can be used temporarily to quickly bring down extremely high blood sugar levels.
And then, there are quite a few patients who have literally no insulin because their beta cells in pancreas are all dead. In such patients there is no option but to give insulin injections. It may be noted that quite often, such patients had been taking sulphonylureas for decades. Sulphonylureas tend to “squeeze” beta cells to secrete more and more insulin. Eventually these beta cells slowly start dying out.(20)
In my practice, for treating diabetes, my philosophy has been always about decreasing blood sugar along with targeting inflammation. My rule of thumb for selecting anti- diabetic drugs has always been in regards to weight loss. Any drug that causes weight gain simply means that it is causing inflammation to go up. So, I use only those anti-diabetic drugs which decrease blood sugar and preferably cause weight loss.
Hence, in my practice, I have heavily relied on Metformin and SGLT-2 inhibitors.
I believe Metformin is one of the best drugs for managing diabetes. Many consider metformin as insulin sensitizer. Many believe that Metformin alleviates insulin resistance. But, that is actually a secondary effect. Metformin is actually a very powerful anti-inflammatory.(21) When inflammation goes down, cells automatically reduce the level of insulin resistance. Insulin resistance going down is thus a result of downsizing of inflammation by Metformin. Due to this, patients actually lose weight when they are on Metformin.(22)
SGLT-2 inhibitors like Dapagliflozin, Canagliflozin, Empagliflozin are also extremely effective anti-diabetic drugs. They don’t do anything to insulin. They simply remove blood sugar by making them flow out of urine. As blood sugar level falls, insulin secretion also goes down. So, SGLT-2 inhibitors actually contribute to decrease in insulin level rather than increasing it. And hence use of SGLT-2 inhibitors lead to quite significant weight loss.(23)
There are also other anti-diabetic drugs that are extremely effective in reducing blood sugar, bringing down inflammation and promoting weight loss.
I have also used pioglitazone in few cases. But I am still not sure. Although it seems it is anti-inflammatory in some tissues, in some other tissues it has pro- inflammatory effects. And since pioglitazone causes weight gain, I tend to believe that pioglitazone might lead to increase in overall inflammation.(24, 25) Although, my notion here might be incorrect because the weight gain in pioglitazone has been shown to be due to water retention and not fat deposition.(26)
In summary, I would like to simply reiterate that one should be extremely careful while using insulin for treating diabetes. Insulin should be used only and only if there is no other choice. I would like to extend this caution towards use of Sulphonylureas as well.
A simple rule of thumb for treating diabetes- Use only those drugs that promote weight loss
What I discussed in this post is not simply my personal view. I have listed all the references for you to verify what I discussed. To make your job easy, let me mention two references that were big eye openers for me. The first one is titled “Insulin Resistance as a Physiological Defense Against Metabolic Stress: Implications for the Management of Subsets of Type 2 Diabetes” that was published by Nolan et al in 2015 in the journal “Diabetes”. This is available HERE
The other reference is another research publication titled “Insulin Therapy Increases Cardiovascular Risk in Type 2 Diabetes”. This publication was authored by Mary Herman and her group in 2017 in the journal “Progress in Cardiovascular Diseases”. If you ever get access to this, please do read.
List of References used:
3. Forbes JM, Cooper ME. Mechanisms of diabetic complications. Physiol Rev. 2013;93(1):137-88.



Very informative and thought provoking article especially for non medicos
The logical explanation of the role of insulin and the body defence mechanism is appreciable
Question remains what could be the approach to manage inflammation not only in diabetics but even the general population who are moving from 40s to 60s . Should limiting the sugar be the only alternative . Doesn’t look appropriate since everything we consume gets converted into some form of sugar . Does taking certain anti inflammation supplements like curcumin or you can suggest something, will that be good to control inflammation?
I have written extensively on this previously.
https://wisethalamus.com/why-are-so-many-young-and-fit-dying-of-heart-attack-and-stroke/
One of the best thought-out and best-written article on the subject. Making it simple without compromising with the science is a very rare skill.
I have been a diabetic myself for the last 17 years and have not started medication. My blood and other parameters are good enough. I have been following a naturopath doctor (Dr Peter D’Adamo) and his blood type diet for about 16 years and now believe that although all human bodies and systems are more or less similar, they are not the same and “one size does not fit all.” For example, some people tend to have higher stomach acid and alkaline phophatase, others tend to have low. Strong correlation between blood types and certain diseases hae often been ignored in many of the otherwise best medical/health researches. Who would in general suspect that some food (certain beans, wheat gluten or dairy) might interfere in glucose mechanism among certain people (Of some particular blood groups)?
Thank you for your excellent and eye-opening initiative!
Thank you for your kind words. You are absolutely right- one size does not fit for all.
Really appreciate you sharing this article.