Table of Contents
Introduction
Today is 4th June 2021. Since Feb 2021, everyday around 0.1 to 0.3 million cases are getting diagnosed in India with COVID-19 and about 3000 are dying. Wave 2 of this pandemic has been a disaster for this country. The best-known institutes are seeing their own best doctors succumbing to this viral holocaust. No one really knows what can save lives. There are theories and expert recommendations- but people are dying anyways.
Recently 20 members of my family and friends (including me) were infected with COVID-19. Initial symptoms started on around 29th April 2021 for nearly everyone. Most of these infected ones were located in a village about 60 kms from the main city, with very difficult access to diagnostic facilities and almost zero possibility of advanced support such as Oxygen/ICU/Ventilator. 12 members of this group were elderly (>65 years age), 4 with relatively uncontrolled diabetes mellitus and 1 undergoing chemotherapy.
By god’s grace, combined with little unconventional approach, the whole family came out of this horrifying ordeal unscathed.
This blog is to document the entire story with the hope that the methodology used might be useful in such resource constrained grim situations.
Disclaimer
I would like to highlight here that the steps what I took to treat my family were unique and were forced due to the extreme constraints I was facing. Also, I am a trained registered doctor with a valid license to practice allopathy. My humble request is PLEASE DO NOT TAKE ANY MEDICINE OR FOLLOW ANY LINE OF TREATMENT WITHOUT CONSULTING YOUR PHYSICIAN.
The Enigma of COVID-19 Disaster: No one can predict or guarantee survival
In Feb 2021, the second wave of COVID-19 struck India with a surprising fury. The mutant strain responsible for this second wave in India seem to be highly infective. While the earlier wave was generally dangerous for elderly population and those with comorbidities, in this second wave even youths and seemingly healthy ones are dying. Around 3000 deaths every day is an alarming number. And when your near and dear ones die, the fear becomes more real. One of my relatives used to work as a doctor in army hospital in Delhi. Last year his mother died due to COVID-19 related complications. This year he got infected and had to be hospitalized. He did not survive. Every friend I know, knows someone who died. Every colleague I talk to grieve about some relative who died due to COVID-19.

With more than 25,000 cases requiring hospitalization daily[1], of course the whole healthcare system collapsed. Almost all hospital beds are occupied, and scores of patients keep running from one hospital to the other to find bed[2]. Finding a hospital bed itself is celebrated with joy and sense of achievement- such is the situation (literally forgetting that hospitalization is just the start of the long struggle). In most cases, access to hospital beds and sustenance is a rich man’s game. Poor people who don’t have such resources just give up. Inside hospitals, lack of beds is just one part of issue. There has been a severe nationwide shortage of “so called” live saving medicines such Tocilizumab and Remdesivir[3]. Similarly, for a long time, there was an acute crisis of oxygen.[2] Many hospitals couldn’t get enough oxygen to support their critically ill patients leading to deaths of many such patients.[4]
Given the nature of emergency, coupled with nationwide sense of panic and dread, black market started flourishing. People have been literally throwing money paying almost 3-4 times higher prices to buy medicines/ oxygen cylinders. There is no guarantee regarding quality when one buys from black market. People have been duped with “fake” Remdesivir vials[5].
But, access to best hospitals and the “so called” life saving medicines gives no guarantee of “cure”.
Thing is no one knows how to really treat. We know that more 90% of those infected with COVID-19 virus in this wave easily recover without any complications. Less than 10% develop complications and require hospitalization.[1] Issue is, there is no way to predict who will be that unlucky 10%. Age and comorbidities might be contributory factors. But if you are young and healthy, still there is no guarantee that you won’t require hospitalization. And once you are in hospital, there is no guarantee that you will survive. Around 10% of hospitalized patients don’t survive.
It is quite concerning to find so many of the top doctors succumbing to this new variant of COVID-19 despite using the best available medical resources.[6] It just means one thing- the current medical science is still evolving and it’s not exactly clear how to save someone from dying due to severe COVID-19.
My Situation: Preparing for the worst
I was based out of the city of Gurgaon since 2018 due to my job at Takeda Pharmaceuticals. When the COVID-19 pandemic started in early 2020 it forced nearly everyone across the world to confine themselves to their homes. I was no exception. Work from home became a norm for most corporates including mine. It gave people like me a unique opportunity to spend a great deal of time with our families. I made full use of this opportunity and within few months I, my wife and my kid shifted from Gurgaon to my wife’s native place near Kolkata.
This place, at the banks of river Hooghly (an arm of the great Ganges), is around 50 kms away from the city of Kolkata. We have quite a large family here staying together with extended family members living close by. For my 4-year-old kid, this shift turned out to be great move with so many people to play with. And for me, work from home is efficient from any place so long as there is decent internet connectivity.
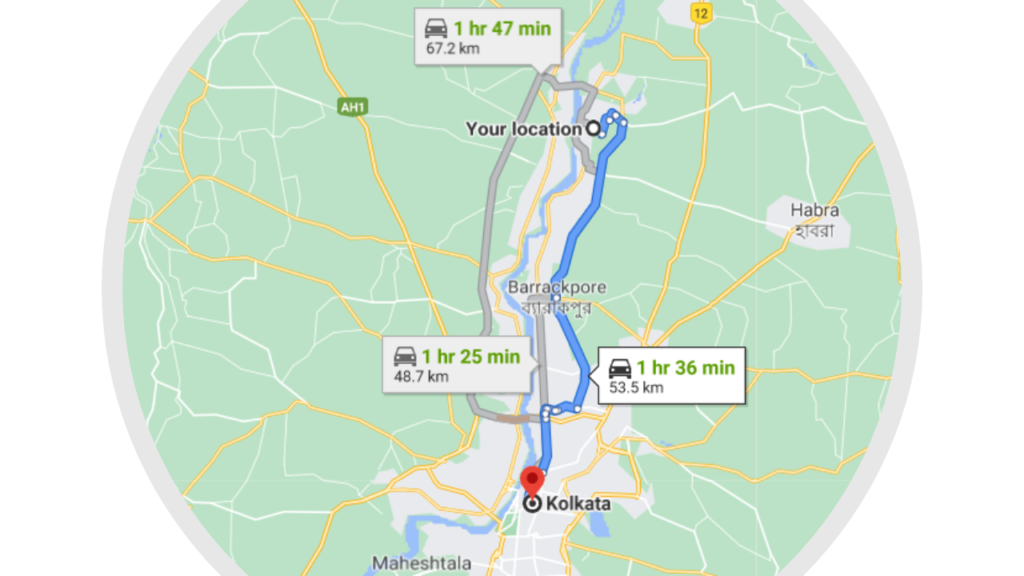
But, being so far off from the main city is highly disadvantageous, especially during this pandemic. There are no hospitals here. The nearest ones are at least 30 mins away if you are driving, and those are not the ones you would rely upon. The diagnostic facilities are not much evolved here- quite basic at best. For consultation, doctors are there. But most sit along a pharmacy with people waiting outside on road. And, in this COVID-19 where best doctors are not exactly successful in solving this enigma, it’s difficult to rely much on the doctors available here. (I must admit here that for most of the established traditional diseases, the doctors here are quite knowledgeable and they really know how to treat. In COVD-19, no one currently is really an expert- there are too many unknowns.)
So, when the second wave started spreading like wildfire, I started my preparations anticipating the worst. And the first step, was to really try understanding the disease in depth. I was at no point under the assumption that I will discover something that no one has. There are much better minds out there. My assumption was that guidelines don’t necessarily incorporate the findings from the latest data. Also, development and release of guidelines is a combination of science and bureaucracy. Also, guidelines assume that you have access to decent medical facilities around. But, my situation was different. I had constraints in terms of access to even basic lab investigations. I had to figure out a way to avoid hospitalization at all costs.
The Science- Understanding clinical course of COVID-19
Since March 2021, nearly every day I was dedicating almost 2 hours reading about latest advances in understanding COVID-19. My focus of study was the phenomenon called “cytokine storm” which is the main reason why anyone dies when infected with COVID-19. This study allowed me to write extensively on the immunobiology of COVID-19 led cytokine storm on this website (I created a 4- parts blog series on this: Part 1, Part 2, Part 3, Part 4).
I won’t go into the details of the virus, the immunobiology and pathogenesis of this weird disease. They are important but will make this article very complicated for a layman to understand.
What I will do is, I will try to explain how the disease starts and progresses and what happens with each stage of progression. This will eventually allow readers who easily understand why what medicine should be used at which stage, and how few medicines can be useless or even harmful if timed incorrectly.
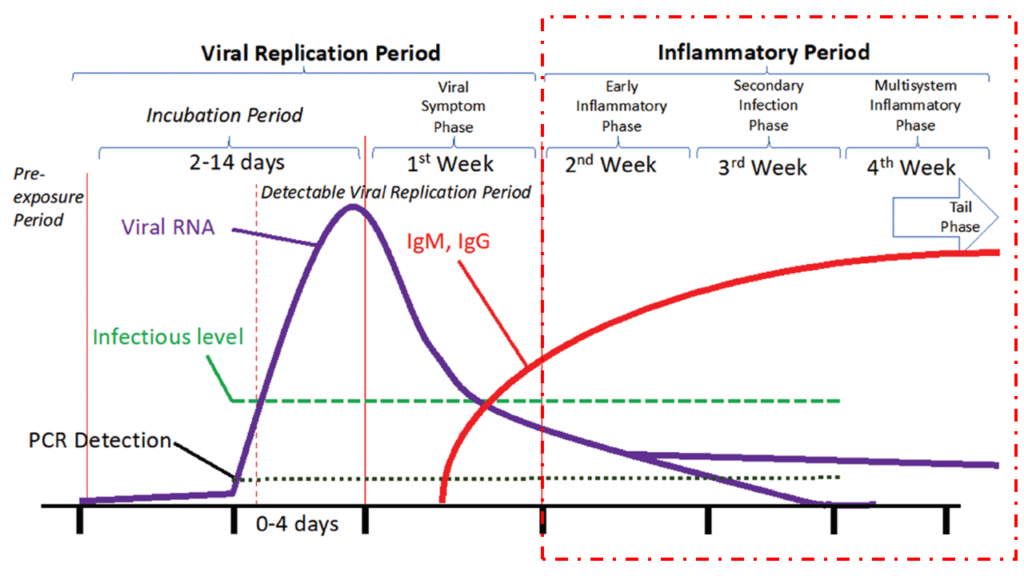
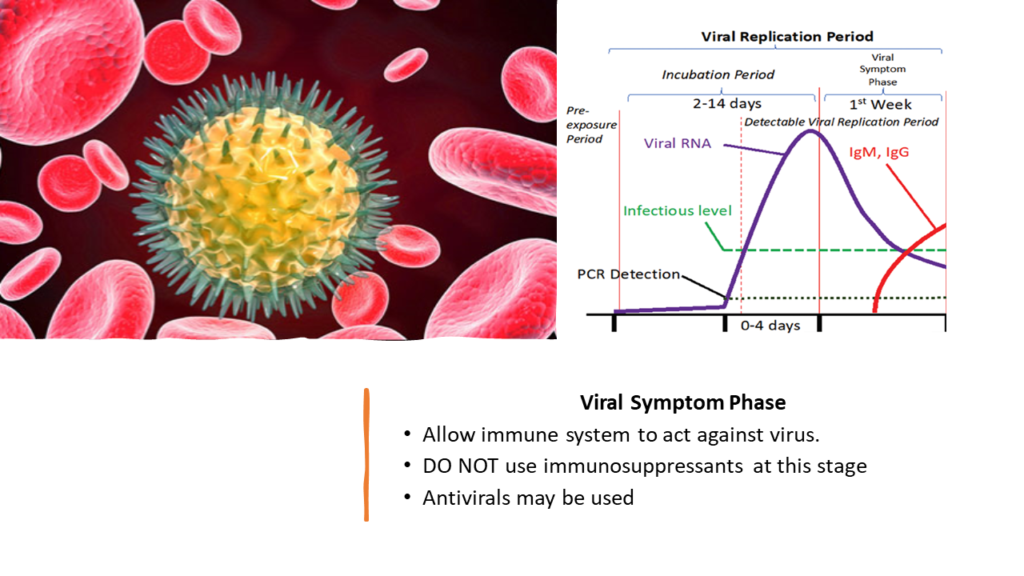
From the time when virus first enters the host, the whole disease course can be divided into two major periods: The Viral Replication Period and The Inflammatory Period [7].
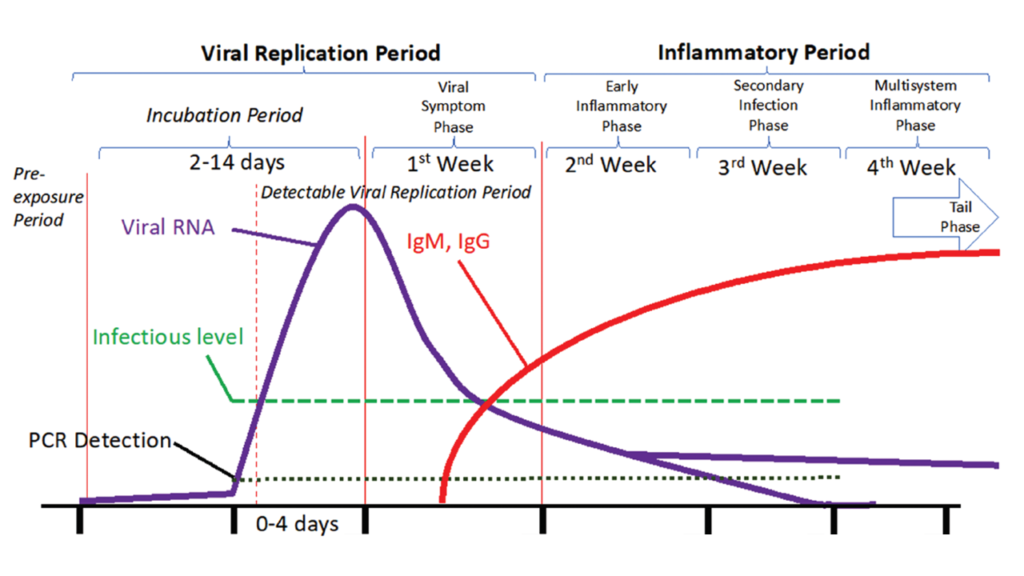
1. Viral Replication Period
This period begins when the COVID-19 virus gains entry into your body. I won’t get into the details of mechanism. The virus particles invade cells of respiratory tract. Each virus particle then uses the infected cell’s machinery to create more viruses. These daughter viruses then come out of that cell and start infecting other cells. This whole process of one virus becoming many viruses and infecting increasingly large number of cells is known as viral replication.
Viral replication period can be further divided into two phases: Incubation Period and Viral Symptom Phase
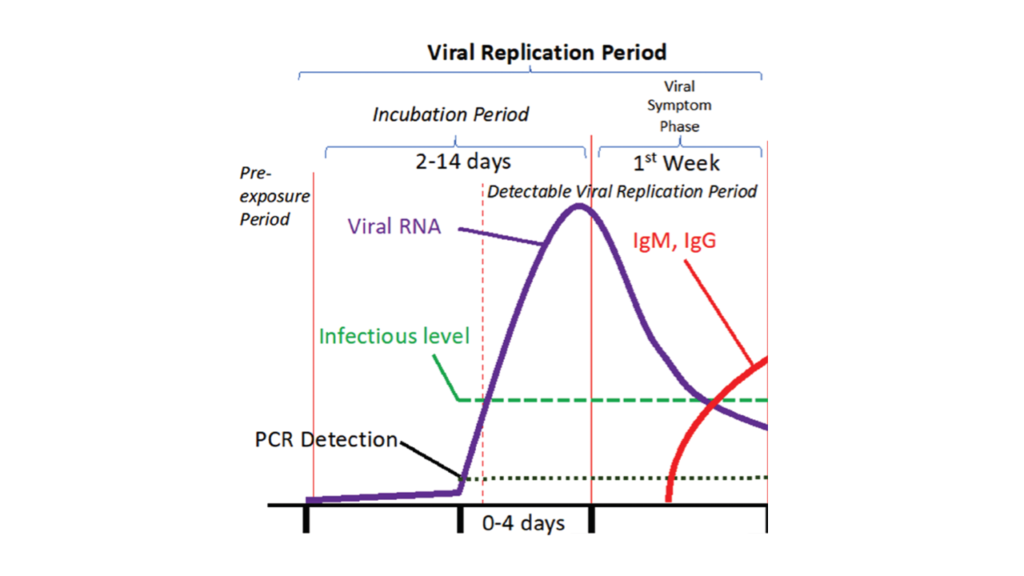
a) Incubation Period
For initial few days while the virus is replicating, the infected person won’t have any symptoms. This initial symptomless phase while the virus has gained entry and is replicating is known as “incubation period”. The length of incubation period varies from one person to another. In some it can be as short as 2 days, in few it can be as long as 14 days.
If you know one is in incubation period, using antivirals might be a great idea. It might significantly decrease the viral load and make the entire disease course mild. But it’s generally impossible to discover if somebody is in incubation period unless there is high suspicion of significant contact with a known patient. From practical stand, I don’t think it’s prudent to start any medicine before symptoms begin. However, there are studies showing role of few medicines such as ivermectin at this stage as prophylaxis. It’s still controversial though[8].
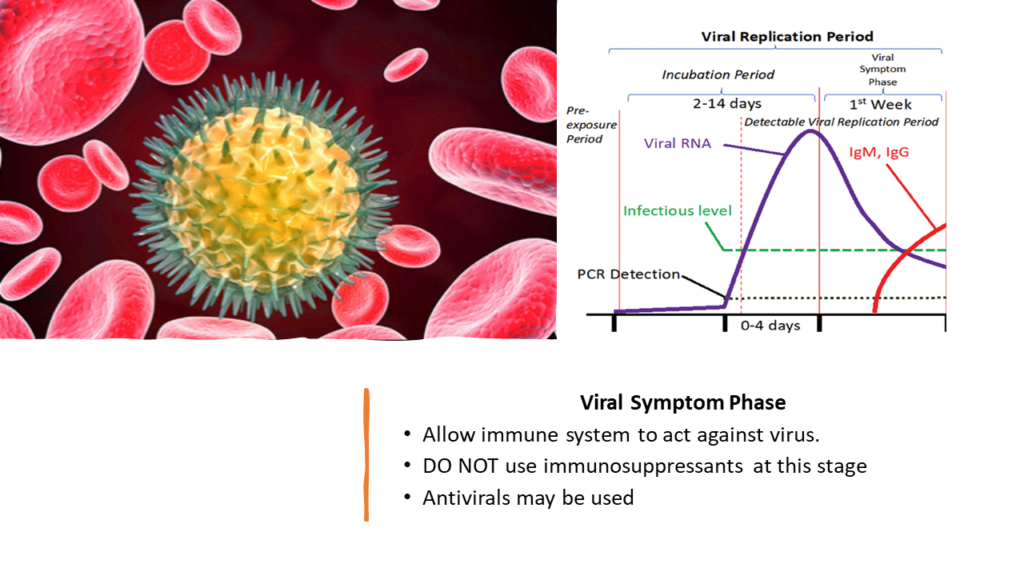
b) Viral Symptom Phase
The end of incubation period is marked by appearance of first symptoms.
The day when the symptoms first appear is the most important day for any patient and clinician from treatment perspective. This day should be marked as ‘DAY 1”.
The most common symptoms displayed by most patients include loss of sense of smell/taste, fever, cough, fatigue, muscle soreness, joint pains, headache, diarrhea, shortness of breath. Of course, a patient will generally have one or more of these symptoms and not all [9] [10]. And around 12% patients remain asymptomatic throughout.[10] Such asymptomatic patients need no medications anyways.
Viral Symptom Phase generally lasts for a week[7]. In this phase, it’s important to allow your immune system to work optimally and eliminate the virus[11]. One might boost this virus elimination by introducing antivirals such a Favipiravir[12]. Ivermectin has also been found useful in suppressing viral activity[13][14]. Similarly, Azithromycin has been reported to have beneficial effects. [15][16]
But what is critical to remember is not to introduce any immune suppressive drugs like corticosteroids at this stage. This will allow virus to replicate uninhibited and might lead to worsening of the disease.[17]
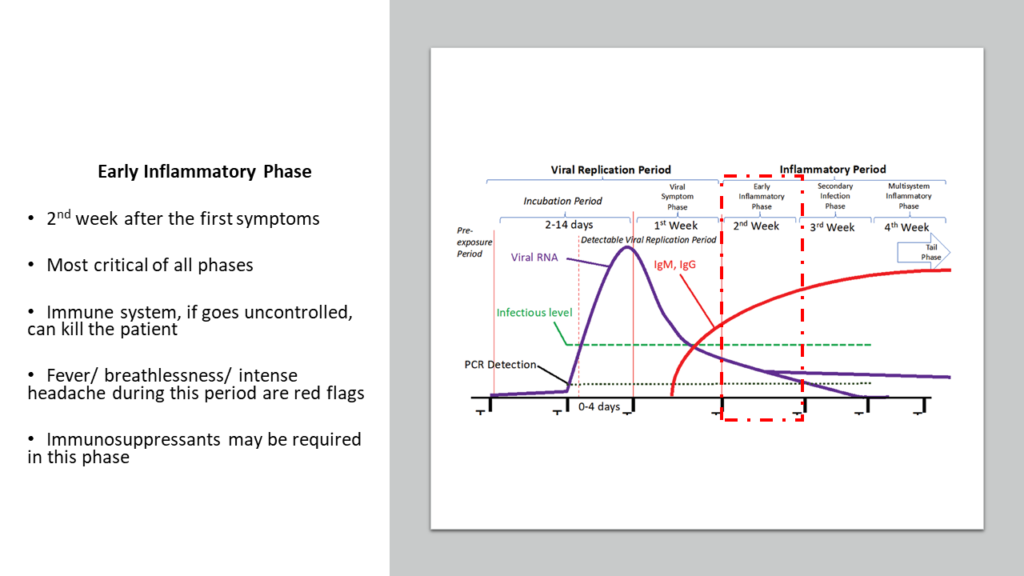
2. Inflammatory Period
Inflammatory period starts from around Day 7- 8 after the appearance of first symptoms. This period lasts for about 3 weeks and can be subdivided into 3 phases- Early Inflammatory Phase, Secondary Infection Phase and Multisystem Inflammatory Phase.
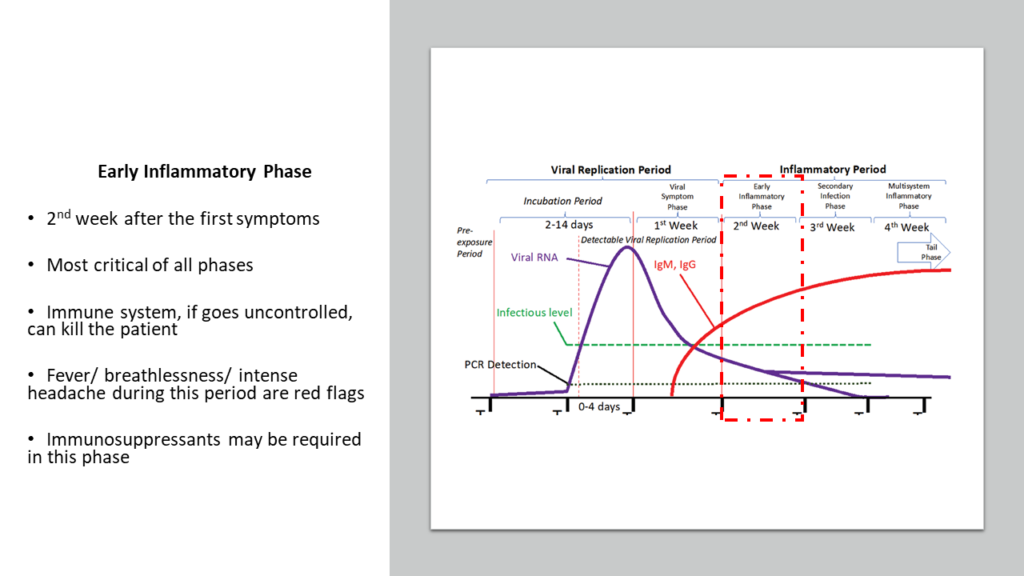
a) Early Inflammatory Phase
This phase exists from Day 7- 8 after the appearance of first symptoms to around Day 14- 15. This second week is the most important period in this disease. What happens during this period and the decisions taken by the clinicians during this period will determine if the patient will survive or not. Actually, majority (more than 90%) will survive this period even without any intervention by any clinician. But the scary part is, there is no way anyone can predict who will progress into that unfortunate 10% zone where hospitalization is needed and eventually might not survive.
This is the period when viral replication is no longer happening, and viral load is generally very low. Virus generally gets adequately controlled by the end of Viral Symptom Phase. But the immune system, which was directed towards killing the virus, is still active and activity keeps going higher.
In majority cases this immune activity, although very high, remains under a certain limit. But in few (around 10%) cases, this limit is crossed. In such unfortunate patients the immune system acts like a mad mercenary who just won’t stop firing. But now there are no viruses to be killed, but only the normal cells of the lungs. If not controlled, the lungs can collapse, and other vital organs will also start getting impacted. This is what we call as cytokine storm and this is exactly what causes deaths.
It’s not the virus, but our own immune system that leads to disaster.
Hence, here antivirals, Ivermectin, Azithromycin etc generally have no role to play. What definitely works here are immunosuppressive drugs such as corticosteroids. Should they be used in all patients? Definitely not. But one must remember that once the cytokine storm starts, its generally difficult for corticosteroids to act and control. It’s generally a matter of chance if they will work adequately. This has been observed in other conditions as well such as bronchial asthma. Corticosteroids are good at preventing an asthma attack if given before the attack starts. But once asthma attack has started, corticosteroids generally don’t work.[18]
Hence, from Day 7 or Day 8 one has be on guard to look out for the earliest signs of deterioration. One of the red flags is continuation of fever or appearance of fever on Day 7 and beyond. This is a good enough indicator to immediately start corticosteroids, and then check blood CRP, D-Dimers, LDH and Ferritin levels to confirm what’s happening. Another red flag is persistent high intensity headache and/ or breathlessness on or beyond Day 7.
b) Secondary Infection Phase
This phase lasts from Day 14- 15 to Day 21, where secondary bacterial/fungal infections start appearing. This is because COVID-19 weakens the immune system. One may now ponder why I am saying COVID-19 weakens immune system while in the previous point it has been mentioned that immune activity is increased. I won’t go into detailed explanation here- but high immune activity doesn’t mean that immune system is healthy. Excessive activation of immune system actually weakens it. To understand in detail what I mean, you may read click here.
Also, during the second week many patients may have taken immune suppressive drugs like corticosteroids. This also might allow secondary infections to proliferate.
So, one needs to watch out for these infections and be careful.
But, if you are out of the second week and still at home healthy, you are out of danger for sure. Yes, there is this scare of dreaded fungal infections such as mucormycosis which have very high mortality rates. But, if you are not hospitalized, have taken just a short 7- 10 days course of corticosteroids, and have kept blood sugar under control, most probably you are safe. I generally advise gargles with lukewarm water mixed with salt at least 3 times daily throughout the disease course of COVID-19 to keep at least oral region disinfected to some extent. I will cover mucormycosis in bit more detail in a later section.
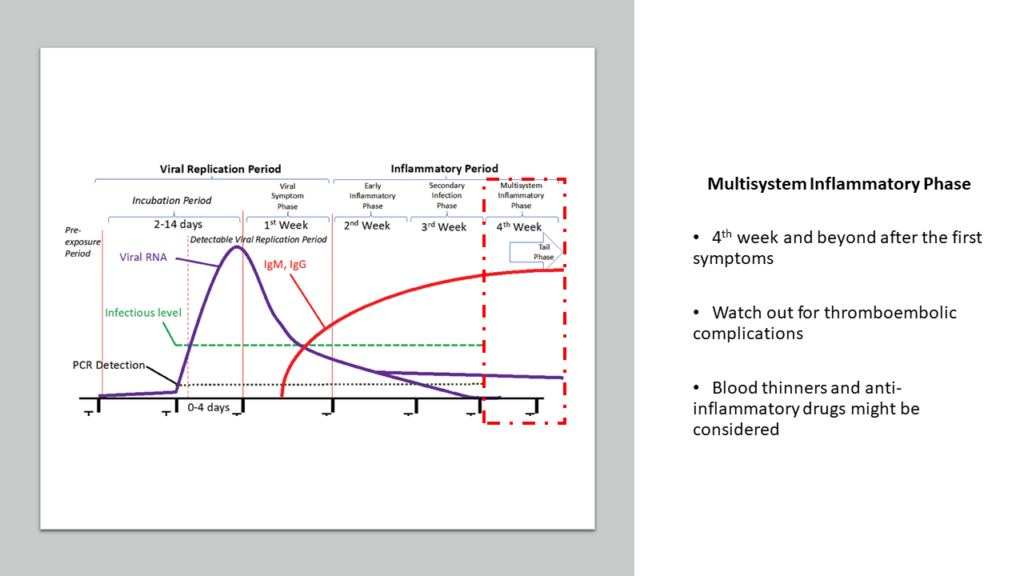
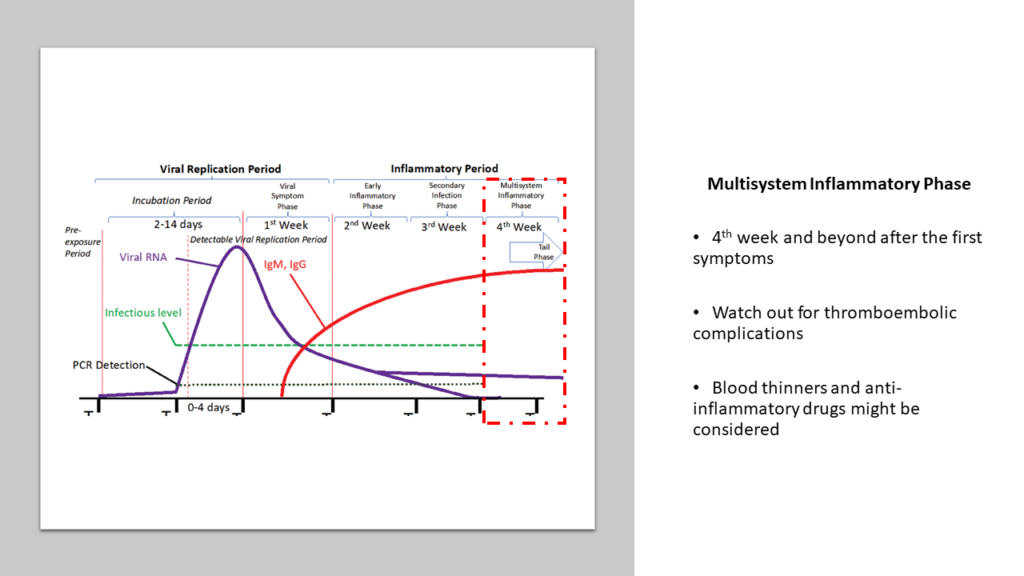
c) Multisystem Inflammatory Phase
This the final fourth week post the appearance of first symptoms. To be fair, this phase can continue for months. This phase is the result of continuous ongoing activity of immune response resulting in a state of constant inflammation. COVID-19 causes immune system to become so reactive that it takes a long time for the immune system to really calm down to its original normal.
It is this constant inflammation that results in prolonged weakness, continued loss of smell/taste etc. How long and how severe this phase will be, depends on how severe was your disease during Week 2. In some, the ongoing inflammation can be high enough to cause critical arteries to become narrow and cause blood to clot leading to episodes of stroke, heart attack etc months after infection. Continued inflammation may alter various organ systems including heart, liver, kidneys, brain and can lead to various troublesome manifestations for several months. Some experts call it as “Long COVID”.
Hence, in lot of patients, it might be prudent to proactively control this inflammation by introducing blood thinners such as aspirin and clopidogrel and use drugs like statins for their anti- inflammatory properties.
Science in action: Facing the nightmare
Nearly everyone in my neighbor was getting infected with COVID-19. And I knew- soon our turn will come. We were all trying our best to avoid. But I was preparing for the worst. I created my own protocol knowing my constraints that I won’t have access to blood investigations or HRCT or oxygen if required. And if things go wrong even for one member, there might not even a hospital bed available. So, my protocol was highly customized to the situation I was in. And I started stocking medicines in accordance with my protocol.
The Start of The Nightmare
It was either 28th April or 29th April 2021. 3 members of my family started reporting body ache, fever and diarrhoea. By 30th April, all 20 members of my family including me started showing similar symptoms. My 4-year-old kid was the only one who remained symptomless and healthy. And strangely, our great grandmother who is 97 years old also remained asymptomatic and healthy.
I was able to get RTPCR report for 4 of them- all were positive for COIVD-19. But here is the thing- if you have typical symptoms you must treat as COVID-19 even if RTPCR is negative. Two of my very close friends in Gurgaon ended up in ICU although both were RTCPR negative.
Nearly all of these 20 members of my family who were infected, were having one or more comorbidities. 12 members of this group were elderly (>65 years age), 4 with relatively uncontrolled diabetes mellitus and 1 undergoing chemotherapy. I am obese with bronchial asthma and borderline Type 2 Diabetes Mellitus. My wife has been on medication since around 6 months now for Chronic Idiopathic Urticaria.
Studies have already shown that although only around 6% of COVID-19 infected patients below the age of 65 years require hospitalization, this percentage is more than 28% for patients >65 years age.[1] And I had 12 such patients with age >65 years. Just by this calculation, around 19% of my family members might end having progressive disease requiring hospitalization- so around 3 to 4 members of the 20 infected might need hospitalization. And this was a conservative figure since I haven’t considered the fact that other members did have several comorbidities. This calculation really got me gripped with fear.
Week 1- Viral Symptom Phase
The first thing to do was to check blood sugar for everyone. I had glucometer for that. My training in diabetes management helped me take care of this part. And depending on individual requirements, I started antidiabetic medications accordingly. It is very important to note that COVID-19 causes inflammation that will anyways cause blood sugar to shoot up. And high blood sugar will impair immune system. Hence, its critical to quickly get blood sugar under control.
Next, I started Favipiravir for everyone. It’s an anti- viral. I also started Ivermectin and Azithromycin. I knew first week would go ok. Fever was under control for most by 3rd May. Only 2 kept reporting fever during day- time, which was a bit concerning.
The Scary Week 2- Early Inflammatory Phase
I was concerned about this second week. This is the time when things go wrong for 10% patients. And for us, this number was 19%- almost double. And I cannot risk even 1 patient going bad, given the constraints I had. With no easy access to blood investigations, it was quite risky to wait for the earliest signs of deterioration and then act. And I already knew that if deterioration starts, it might be a bit too late for corticosteroids to act[19]. Based on these, I had already made a decision while making my protocol.
Rather than waiting for deterioration to happen, I had planned to preemptively strike the immune system with corticosteroids.
I knew that this is a bit controversial. But, given the constraints, I also knew it was the right thing to do. And logically it actually made sense even in normal scenarios (although many might oppose this saying its abuse of corticosteroids). The logic is that by Day 6 or Day 7, your immune system has already taken care of the virus. After Day 7, it’s your immune system which will end up killing you if you are unlucky. And there is no way to know if you will be lucky or unlucky. So, why not proactively silence immune system from Day 7 for all cases? Why to take chances?
The currently used protocols are definitely scientific, but not good enough I feel. Else so many deaths wouldn’t have happened due to cytokine storm. Even the best of the institutes is not able to save many, despite the best available facilities. Many of the top doctors have succumbed. Fact is we are still learning about this disease and no one really has complete answers. So, if we know that in few patients immune system will go berserk and we cannot predict who are these few, why not give a short course of corticosteroids in all patients from Day 7? This view is actually supported by several experts globally as well, based on the logic as well as available data.[19][20][21][22]
Some might say such use of corticosteroids will increase chances of infection. Some might say it is such abuse of corticosteroids that has led to emergence of fungal infections such as mucormycosis. But here is my argument. Across the world millions of patients have been taking corticosteroids daily for decades for various conditions such as autoimmune diseases. Forget corticosteroids, thousands of patients across the world have been taking drugs like Tofacitinib for years [23]. Tofacitinib is much more potent immune suppressant than corticosteroids. Of course there are side effects when you take such medications for years, but they are all manageable[24][25][26]. Here, in this COVID-19 infection, all I am suggesting is a short 7 days course of corticosteroids and then no more of it. How can this be more harmful than risking the possibility of hospitalization and death still beats me.
Anyways, given the challenges I had, I knew I must use corticosteroids proactively and preemptively cull off any chance of cytokine storm.
6th May was Day 7 from first symptoms for nearly all of us. This is when I started corticosteroids for all, both oral as well as via inhalers. Inhaled corticosteroids directly act at the site where inflammation is occurring majorly while oral steroids work take care of the immune system activation in general. The other drug I started was a combination of Atorvastatin 20 mg, Aspirin 75 mg and Clopidogrel 75 mg once daily. Vascular impact of COVID-19 is well documented. Many experts across the world believe that COVID-19 should be considered as a disease of blood vessels rather than a lung disease.[27][28][29] Statins like Atorvastatin also decrease risk of progression of COVID-19 infection into cytokine storm.[30]
The next seven days I kept a close watch on everybody’s blood sugar given the fact that few might experience sudden spike because of introduction of corticosteroids. 2 of the 20 did witness such rise, which was quickly controlled with altering medication dose of anti- diabetics.
These 7 days were amongst the most anxious days of my life. Nearly every day I would hear someone in my neighborhood succumbing to COVID-19 and I would keep getting tensed. I had two members whose fever kept coming till Day 8. Then one started reporting no fever. The other member kept reporting fever till Day 10. For him, I was able to get blood investigation reports for inflammatory markers such as CRP, D-Dimers, LDH and Ferritin. Luckily, fever stopped in next 2 days, never to return again.
Slowly, but safely, we finally reached 14th May. No was reporting any fever or breathlessness. I had already started tapering down the dose of corticosteroids. The corticosteroid inhalers were completely stopped.
After Week 2
By 16th May everyone was complete off all corticosteroids. What was still continuing was the combination Atorvastatin 20 mg, Aspirin 75 mg and Clopidogrel 75 mg once daily and this shall continue till 15th June. This is to cover the last phase- the Multisystem Inflammatory Phase and prevent any delayed vascular complications seen in so many patients, months after infection.
Since Day 1 I had made it mandatory for everyone to do gargles with lukewarm water mixed with salt, thrice daily. We are still continuing that. The chloride ions from salt is a power anti-bacterial and anti- fungal, and might protect against secondary infections.
It’s now well more than month since COVID-19 attacked us. I can safely say we prevailed. I would love to believe that the customized protocol that I made worked, and it’s a good protocol if you have constraints similar to what I had. But that would actually be too tall a claim for science. Science requires a structured randomized control trial in a significant number of patients to test if this protocol is really effective and safe. Till such evidence is gathered and documented, I will have to accept that I might have been immensely lucky that all the 20 members of my family (including myself) came out of this COVID-19 scare unscathed and safe.
Worst case scenario readiness

What if even one member would have deteriorated into an uncontrolled cytokine storm? This was the biggest fear I had. My all efforts were towards ensuring with 100% accuracy that not even a single patient deteriorates. Because that would have been a complete disaster. I know I am repeating- but we had no access to any oxygen cylinder or any hospital with ICU/ventilator. Even the biggest cities were facing challenges of hospital bed availability with seriously ill patients running helplessly from one hospital to another.
But what if my protocol was not 100% fail- safe and someone deteriorated? I was cognizant that this was also a likely scenario and I had to be prepared to face the same as well. I needed to find and stock medicines that were oral and readily available.
I had a very recent experience with 4 COVID-19 patients admitted in ICU at my friend’s hospital, around a month back. All were having oxygen saturation hardly maintained above 70% on ventilator. CRP, D-dimers, LDH, Ferritin all were way too high indicative of uncontrolled cytokine storm. My friend was searching for Tocilizumab so were the troubled families. But Tocilizumab was not available anywhere. Based on our knowledge of immunology, we decided that Tofacitinib might work as good as Tocilizumab. And many of my friend’s patients with rheumatoid arthritis were already on Tofacitinib. So, as an educated risk, Tofacitinib was started in these patients. One patient responded within 24 hours with CRP falling dramatically and oxygen saturation rising. Other 3 patients also started responding. By next 2 weeks, all the four patients were discharged- they all had recovered. I have also talked about this in another blog.
This was no miracle, but pure science. Tofacitinib is a powerful immunosuppressant. Its oral. It was readily available, because not many doctors in India knew about it at that time. Now slowly this knowledge is catching up. It’s also in COVID-19 treatment guidelines published by Gujarat Immunology Society.
The same guidelines by Gujarat Immunology Society also talks about use of Colchicine to fight cytokine storm. I did my own research. Available data on Colchicine is quite convincing. [31][32][33] It is also oral and quite readily available.
So, I went ahead and bought several strips of Tofacitinib and Colchicine. I was prepared for the worst now- at least somewhat prepared. Luckily, I didn’t have to use to them.
Implementation Challenges
Lack of access to basic medical/diagnostic facilities was a critical challenge to start with. Then was the enormous challenge with currently used protocols which couldn’t give 100% assurance that no patient will reach hospital.
But the biggest challenge was something I hadn’t imagined. When I started treating this herd of 20 patients, I realized that apart from few common medications each patient had his/her own set of different medications. For example, there were diabetes patients, and each had different medicines with different dosing and schedules.

So, I had to prepare an excel to note which patient takes what medicine at what dose and at which time. Then I had to set reminders on my phone so that I don’t forget. Then, I had members who would challenge me on every medicine that I would give. Many would shudder by the fact that I was giving them corticosteroids. The sheer effort of convincing each in layman’s language was maddening. More so, when I myself was rendered weak by COVID-19.
The sheer frequency of reminders and then pushing each to take the medicines was really hectic. But eventually it all worked out.
Will I use this novel protocol in for all patients?
Till date I have treated 49 patients with COVID-19. No one experienced deterioration. I must say- have been really lucky till now. 20 of these are my family members (including myself) from the above narrative. In rest of the 29 patients I didn’t have to face the challenges in terms of access to facilities. In them I used the clinical course during the first 7 days as my yardstick to judge if the patient will deteriorate. For example, if someone had fever or any other red flag symptoms on Day 6, I would quickly order for blood investigations to check if parameters like CRP, D- dimers, LDH or Ferritin are high. If so, then I would immediately commence short course of corticosteroids. If someone on Day 8 reports high fever, I don’t wait for blood reports. I do order them, but I start corticosteroids concurrently. If reports are normal (which haven’t been so even in single such instance), I can stop easily immediately.
The issue with this approach is that there is a chance that you can get a bit too late in preventing cytokine storm from going beyond control. I personally believe that if the blood reports are showing bad signals, it will be anyways challenging for corticosteroids to act and bring things to normal. Sometimes the patients report back late. They might come on Day 10 to say that they have had high fever since past 3 days. It’s generally too late by then.
And I truly think this is the reason why so many patients end up into hospitals and some don’t survive. In trying to predict and then act, sometimes it becomes too late to act.
CD4:CD8 ratio- A predictive tool to guide treatment choice
I have written extensively about the use of this ratio as a simple predictive tool to determine who will deteriorate if infected with COVID-19. You may click here, if you wish to read about it in detail.
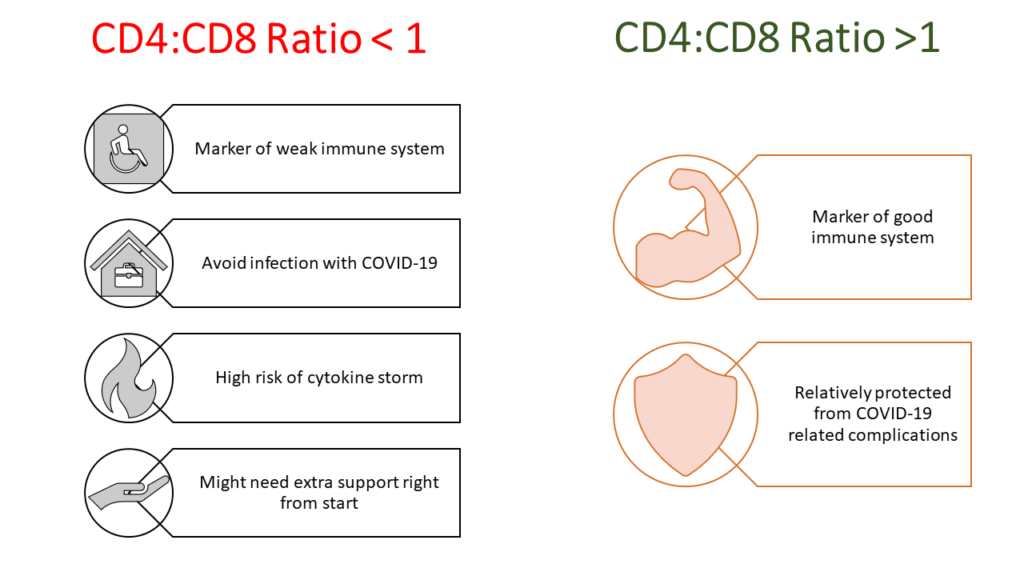
This ratio is an ideal guide in terms of deciding in which patients you will definitely start corticosteroids from Day 7. This ratio should be ideally done for everyone irrespective of whether someone is infected with COVID-19 or not. If someone has this ratio less than 1 and he/she gets infected, in this person I will definitely start corticosteroids on Day 7. I won’t wait for any red flags, I won’t wait for any blood investigations.
If someone has this ratio more than 1, I will most probably never have to use any immune suppressive drugs. I will reserve using corticosteroids in such patients only if red flag signs like fever appear and blood investigations how CRP, Ferritin etc are going high.
But without such early warning system like CD4:CD8 ratio, it is really risky to wait for things to go bad and then start corticosteroids. However, for external patients, its challenging for any doctor to go against guidelines.
What about pulse oximeters?

In this customized treatment protocol that I used for my family, you must have noticed that I haven’t mentioned anything about oxygen saturation or use of pulse oximeter. It was deliberate. I think uninformed use of pulse oximeters have been a real source of panic, and within the complexity of my situation, panic was one thing I really wanted to avoid. Let me explain my stand.
Pre COVID-19 pandemic, most of the people hadn’t even heard of this device called pulse oximeter. Even asthmatics like me didn’t ever had any pulse oximeter at home, and neither was ever recommended by any doctor. During my training as a doctor, we used pulse oximeter only in few hospitalized patients when needed- it was never used in OPD.
And today, nearly every house has pulse oximeter. Google and Whatsapp has anyways made an “expert doctor” out of every common man who knows how to read.
I know someone very educated but with no knowledge of any relevant biology, vehemently arguing about why antibodies need to be tested before vaccination. He had no clue about any concepts regarding IgG or IgM and used google to decide that CDC guidance is incorrect. After 30 mins of wasting time, I had to literally tell him to either trust an expert and don’t argue or just trust google and don’t seek any expert opinion. I also see even lot of doctors resorting to google knowledge rather than going through actual data and understanding science. I understand many might not have time or even the required expertise to analyze data. In that scenario, the best option then is to just follow published guidelines by trusted medical societies.
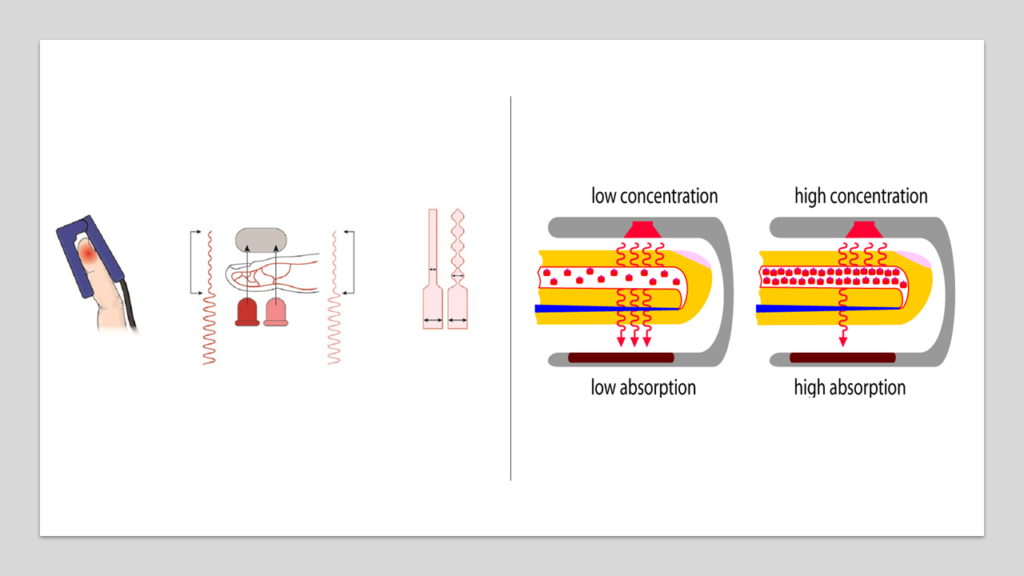
Mechanism of Pulse Oximeter
An oximeter generates beams of light that pass through the blood in the finger. Oxygenated and deoxygenated blood absorb these waves of this light in different amounts. By measuring changes of light absorption in oxygenated or deoxygenated blood, the device is able to measure the amount of oxygen in blood. A strong, regular pulse is critical for oximeter to give accurate readings obtain a good signal and accurate reading.
Fallacies with pulse oximeter one needs to remember
There are few critical points that one must note about pulse oximeters[34] [35]:
- Oximeter reading may be inaccurate if you have artificial nails or are wearing nail polish or your fingernails are dirty.
- If the pulse is weak (which is true in frail/old people), oximeter will give inaccurate results
- Difference in skin pigmentation can lead to different readings in different individuals for same amount of oxygen saturation- especially in those with darker skin.
- External light sources potentially can influence the readings. One way to mitigate this issue is to use an opaque cloth or rubber wrapped around the probe to reduce the external light reaching the light detector
- Movement of body parts can cause errors in readings
- Hemoglobin is the pigment in blood that confers red color to it. This hemoglobin can exist in various forms and has direct impact on accuracy of any oximeter. For example, excess of carbon monoxide can lead formation of carboxyhemoglobin which falsely elevates the oxygen saturation values measured by pulse oximeter. Similarly, changes in quantity of methemoglobin (another form of hemoglobin normally present in our blood, representing close to 2% of total hemoglobin) can impact accuracy of oximeter readings. Higher levels of methemoglobin cause a pulse oximeter to generate readings closer to 85% regardless of the true level of oxygen saturation
The above list of possible fallacies is not exhaustive.
As you can see, there are too many variables that impact accuracy of any oximeter. Also, the assumption is that the oximeter we use is generating accurate readings. But even this assumption might not be true- the oximeters available in the market might not be really accurate at all.

In US, pulse oximeters are prescription medical devices. What it means at the end is, in US you will get pulse oximeters which have been certified by US-FDA for their accuracy. In India, we have no such system. Most of the ones that are sold in shops or online are “made in China” and there is no way to say for sure if the readings are accurate.[36][37] In fact studies are now showing that many of these easily available oximeters in India are actually of poor quality with high level of inaccuracy. [38]
Interpreting readings from oximeters and correlating the same with patient’s condition is purely a clinical task and can be done only by a trained doctor. Moving this decision making from doctors to patients is a good recipe for disaster. Lack of complete knowledge about the fallacies with oximeters and inaccurate low-quality devices has will only lead to inaccurate decision making from patients’ ends.
I have had patients within my family arguing with me on my clinical decisions based on their understanding of oximeter readings. And it’s really impossible to explain everything with completely honesty and science to every patient, most of whom have no idea about anything close to human biology. It takes more than 5 years of dedicated training for a doctor to have some understanding of how human body functions and how medicines work, and translating this knowledge into layman’s language within 10 minutes is not genuinely possible.
I would like to share one interesting experience. Few days back a patient approached me who had nearly recovered from COVID-19. She had very mild disease. It was around Day 13 for her, and she had no fever since Day 4. She came to me because her oximeter was showing 89. She had no other complaints. There was no breathlessness, no fever. I asked her why she checked her oxygen saturation. Her reply was that she was just checking because she had an oximeter at home. Now as per current guidelines, she should be immediately hospitalized.[39] But my clinical side told me everything was ok and there was no need. Just to be on safe side, I ordered for blood reports and HRCT. She got all these done with extreme difficulty and had to travel quite a bit for this. I felt bad- but I had to be sure.
All reports came normal. It was surprising, though I had expected it. I made patient to literally jog a bit to see if there were any signs of low oxygen. She was actually fitter than me!
Then something occurred to me. I asked patient to rub her hands vigorously and then use oximeter. It now showed 97.
My advice regarding using oximeter
If there are no red flags (fever, breathlessness etc), oximetry is of little value if done by a patient. Such practices will only result in inaccurate decisions. If you do have fever after Day 6 or Day 7 of COVID-19, maybe then oximetry becomes a good way to decide when to think of approaching a hospital. In general, oximeter readings should be interpreted by a trained doctors and clinical decisions should be based on his/her medical judgment.
Few words on Mucormycosis- The Black Fungus
I will be soon writing a detailed blog on this. But there are a lot of myths floating around, around this topic and it becomes quite important to quickly clarify few of them.
What is Mucormycosis?
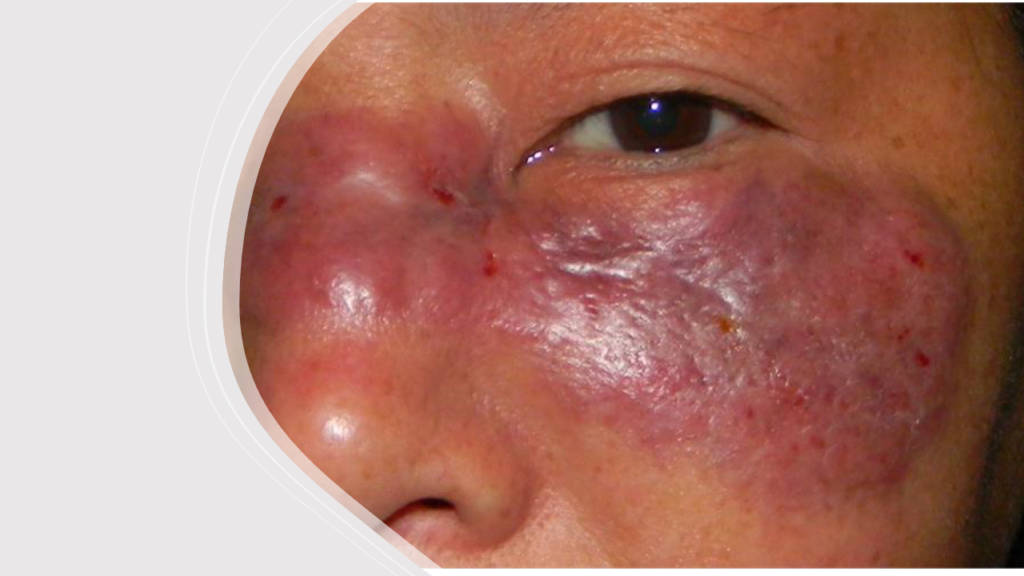
Mucormycosis is a severe fungal infection. It is caused by a group of molds called mucoromycetes, which is a saprophytic fungi of the order Mucorales.[40] Rhizopus arrhizus is the most common mold causing mucormycosis in India and globally.[41] This fungus feeds on iron in the blood, eventually destroying the blood vessels. As the blood supply gets cut off, the tissues which depend on those blood vessels die off. Slowly but surely the area of invasion keeps growing and as the fungus keeps destroying the blood vessels more and more tissues keep getting destroyed.
Is it a new disease like COVID-19?
Mucormycosis is definitely not a new disease. It was initially described in 1885 by Paltauf, and was known by various names including zygomycosis and phycomycosis. [42]
We, in general, never really heard of this because it’s actually pretty rare.
Is Mucormycosis unique only to India?
No. Mucormycosis is seen across the world. But since we are the world’s largest population in the world, its statistically obvious that India would contribute to a very high number of cases. Globally the incidence rate of mucormycosis is about 0.005 to 1.7 per million population.[43] However, more than 70% of the cases are reported from India. India actually reports highest burden of mucormycosis in the world with an estimated prevalence of 140 cases per million population.[44]
Is rampant use of Corticosteroids responsible for this?
Out there, there are almost millions of patients (due to various conditions such as rheumatoid arthritis etc) have been taking very high dose of corticosteroids every day for decades. Mucormycosis was never a significant concern there.
Forget steroids, there are thousands of patients on much more potent immunosuppresant called Tofacitinib- taking daily for years. Again, mucormycosis was never so high a concern.
So, immunosuppression, although one of the factors, can’t be responsible for this current mucormycosis epidemic
Why are we then seeing so many cases on mucormycosis with this COVID-19 pandemic, and that too mostly in Indian patients?
There are many factors responsible for this. First thing to remember is that COVID-19 infection itself makes us susceptible to opportunistic infections like mucormycosis. In majority of the cases, there is significant loss of defense cells called lymphocytes (medically this loss of lymphocytes is known as lymphopenia). This lymphopenia is more pronounced in patients developing severe COVID-19. [45] [40]
It is also an interesting finding that the fungi causing mucormycosis make use of a receptor called GRP 78 present in our blood vessels for launching its attack. And GRP 78 has been postulated as one of the receptors responsible for SARS-CoV-2 entry. [44]
Fungi feed on iron. They proliferate on the iron available in blood. In COVID-19 the amount of available iron in blood rises. More the severity, more is the available iron. This “available” iron is also reflected by the fact that severity correlates with serum ferritin levels.[46] Similarly, diabetes also leads to increase in iron availability to fungus. [47]
It’s obvious from the above points that it’s the severity of COVID-19, rather than anything else that is the main cause of this rising menace of mucormycosis. Patients with uncontrolled diabetes definitely have a higher risk. Immunosuppression definitely also contributes to this risk. But I definitely don’t believe that a short course of corticosteroids would play any significant role.
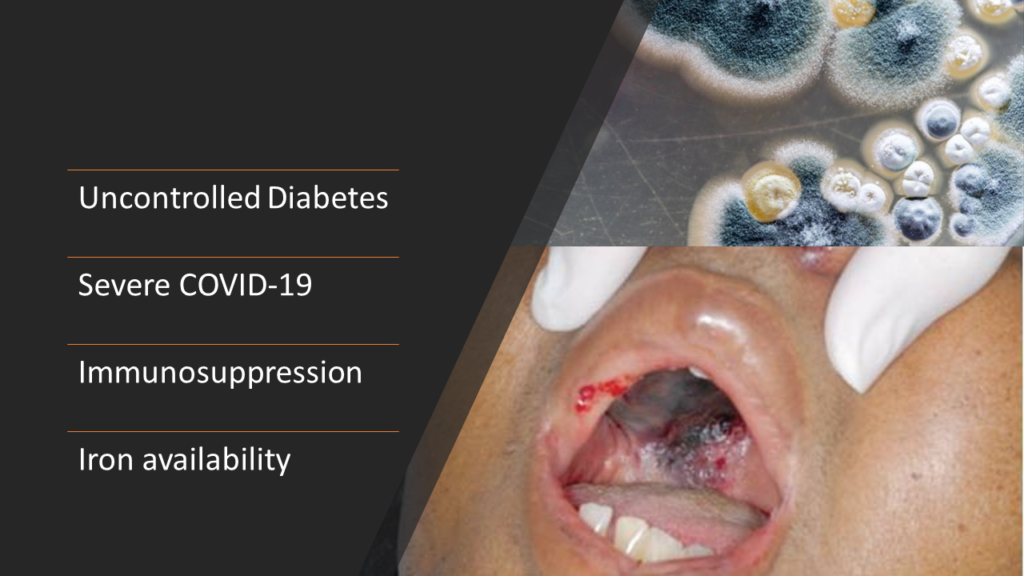
We already discussed that India being the second largest population in the world, if COVID-19 infection causes increase in mucormycosis, its natural that India will contribute to amongst the highest number of mucormycosis cases in the world. Moreover, India is already considered a diabetes capital of the world. [48]
Are the oxygen cylinders and the humidifiers responsible for increased incidence of Mucormycosis in India?
We just have hypotheses here and nothing scientifically proven. But there are few pointers to ponder on. We have seen much higher incidence of mucormycosis in India during the Wave 2. Iron is an essential component for mucormycosis. India might be the only country which has diverted iron industries during Wave 2 to produce and supply oxygen. There iron cylinders come from various sources and lay stacked up in damp unhygienic conditions which are actually ideal for any fungus to proliferate. And the spores will continue to exist, theoretically, even if these cylinders are then filled with oxygen. Is this the reason behind epidemic? Possible, but can’t say for sure.
Most cases have been seen in patients who had been admitted to hospital and taken oxygen. So, is the source of mucor spores these oxygen cylinders? Possible, but again can’t say for sure. Oxygen from the cylinder goes through a humidifier before reaching the patient. The water used in this humidifier, if not clean, might theoretically contain fungi and can enter the patient. Again, nothing is proven.

My personal opinion is that fungi and their spores are in the air. If you are susceptible, you don’t need any special source like oxygen cylinders to infect you with fungi. The reason why it’s so commonly seen in hospitalized COVID-19 patients is the very fact that you will be hospitalized if you generally have severe COVID-19. And we saw earlier that susceptibility to mucormycosis correlates with severity of COVID-19.
Is Amphotericin B the only way to treat this? Are there any alternatives?
Mucormycosis infection is scary- scarier than COVID-19 itself. Across the world, case fatality rate with mucormycosis is close to 50% [5]. Issue is mucormycosis is very difficult to diagnose. By the time it gets diagnosed, its generally too late. Early diagnosis and treatment are essential. A delay of even 6 days is associated with a doubling of 30-day mortality from 35% to 66%. And even if its diagnosed early, prognosis for recovery from mucormycosis is poor despite aggressive combined surgical and medical therapy.[43]
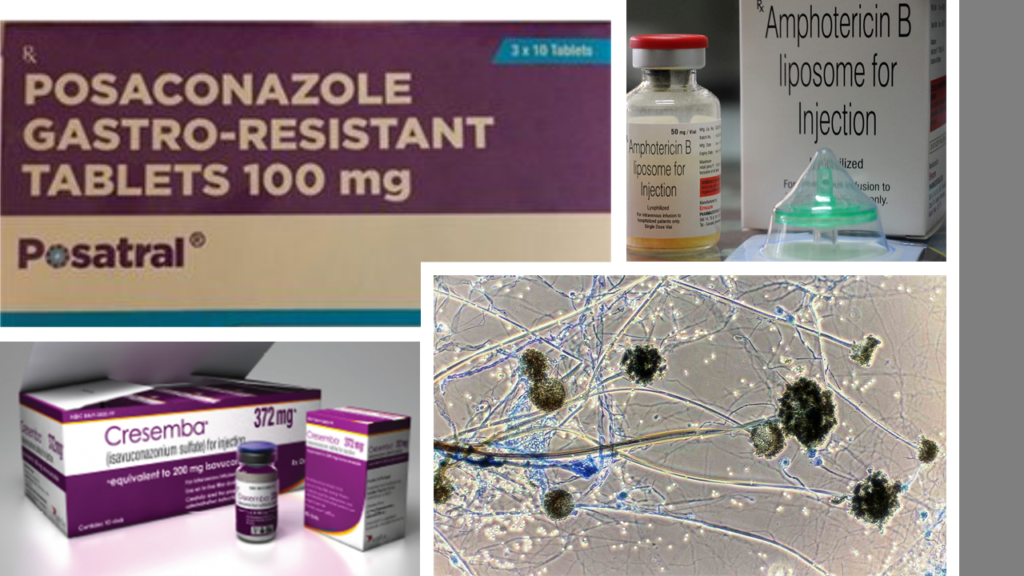
Amphotericin B has been widely recognized as the only drug that works against mucormycosis, along with surgery. And this is true to a large extent. Due to this, there is today an acute shortage of Amphotericin B across India. And with Amphotercin B things are not that simple. It itself is very toxic to kidneys and some really don’t tolerate this drug. Of course, there are alternatives like Posaconazole or Isavuconazole. But Amphotericin B remains the most effective solution.
In my situation of extremely limited access to any resources, I was also scared to death of the possibility someone in my family contracting mucormycosis. To start with I already had 4 patients with uncontrolled diabetes. And I had put all under oral corticosteroids from Day 7, due to the reasons I explained. Although I knew that short course of corticosteroids couldn’t invite mucormycosis infection- but what if I was wrong? But then, my priority was to prevent cytokine storm. And if that objective is met, it means no one then gets severe COVID-19. And it’s the severity of COVID-19 that has direct correlation with chances of mucormycosis infection. Next, I also had ensured the everyone’s blood sugar is well below the normal limits including in those 4 who had very high blood sugar levels at the start.
Still, fear lingered. And I once again resorted to understanding the disease in depth by scanning all the available literature. Even a single case of mucormycosis and its game over for me since I won’t have access to hospital or Amphotericin B in this resource constrained village 60 km away from the main city. I was searching for medicines beyond Amphotericin B, preferably oral and was easily available.
Posoconazole is oral and not really scarce. But it’s not that effective as Amphotericin B. So, it was one medicine in my radar. But what really got me excited was when I discovered that maybe we can used “scorched earth policy” against mucormycosis.
Scorched earth policy is a military strategy which involves destroying anything that might be useful to the enemy which is advancing through an area. All of the assets that can be used by the enemy are made useless or unavailable, such as food sources, transportation, communications, industrial resources, and even the people in the area. In 1941, when Germany attacked Russia, Russia was unprepared to counter that invasion. They did try to put up some resistance, but Germans were too powerful and couldn’t be stopped. It was then Stalin adopted “scorched earth policy”. The philosophy was- a hungry enemy with no resources can’t invade much. Essentially, the Soviet troops burned their own crops, destroyed bridges, and evacuated factories in the face of the German advance. Entire steel and ammunitions plants were dismantled and were shipped away from the German reach. Even the rail system around the path of German advance were destroyed. The scorched earth policy created severe problems for the German war machine which was trying to keep her three million soldiers supplied with the necessary food and ammunition.[49]
So, is it possible to starve this fungus if I cannot kill it?
And the answer is- maybe YES. We earlier discussed quite in detail that the mucoromycetes (the fungi causing mucormycosis) feeds on iron present in blood. If this is made unavailable, mucormycosis cannot spread. The central role of iron as primary requirement for mucormycosis infection leads to the theoretical possibility of utilizing effective iron chelators as adjunctive antifungal therapy. When tested in labs, it has been conclusively shown that iron chelators like Deferasirox did not allow the mucormycetes to take up iron, ultimately killing the fungus.[50] When administered to diabetic mice and mice with compromised immunity infected with mucormycosis, Deferasirox significantly improved survival and decreased tissue fungal burden, with an efficacy similar to that of Amphotericin B.
A 2011 study showed how compassionate use of Deferasirox helped cure 7 patients with mucormyosis in whom complete debridement was not possible.[51] Patients seriously infected with mucormycosis and not responding to Amphotericin B might respond and get cured if Deferasirox is added. [52]
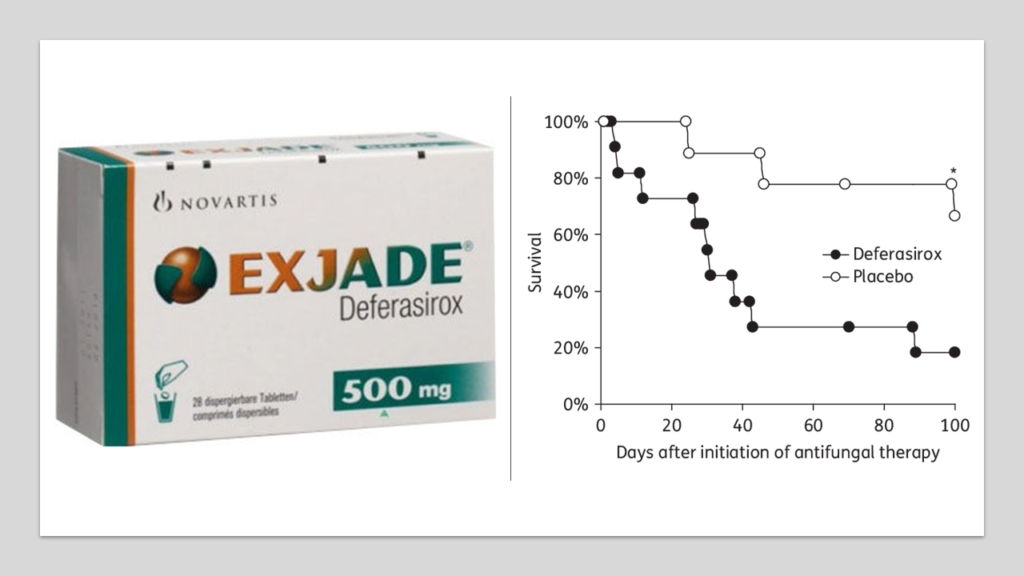
Deferasirox is oral. Its easily available in India. Posoconozole is also oral. And, the above data makes me believe that, if there is no access to Amphotericin B, Deferasirox may work miracle when combined with Posoconazole. If someone would have reported sinusitis, or nasal block or some form of facial pain, I would have started this combination. And this was my strategy, in case of an unfortunate encounter with mucormycosis.
I have to make a humble declaration here- I have no idea if Deferasirox + Posoconazole works in mucormycosis. I have no experience. I was lucky that no one got this scary mucormycosis infection. The combination I am suggesting maybe tried in extreme situations when you have no access to any hospital. And again, you would need a doctor’s supervision.
Concluding remarks
I really feel I was extremely lucky that all of the 20 members of my family (including myself) came out of this COVID-19 infection without any complications, despite all so many comorbidities. I could do blood investigations for inflammatory markers only for 1 patient. I did not do any HRCT for any patient.

In the hindsight, I really think it was the right decision to proactively start a short course of corticosteroids from Day 7, given the challenging situation we are in. However, I don’t do this with other patients as a routine and wait for some red flag signs.
I personally feel that a short course of corticosteroids from Day 7 is a safe way of eliminating any chance of cytokine storm in any patient infected with COVID-19. It’s too risky to allow things to go bad for the patient and then start corticosteroids. It’s generally a bit too late and its purely a matter of luck if patient with respond- most will respond since we already know that only 10% progress into severe disease. But there is no way to guarantee that one won’t fall in that unfortunate 10%.
I don’t think such a short course of corticosteroids puts any patient in risk, given the fact that there are so many patients taking corticosteroids every day for decades.
Mucormycosis is really scary. There are lot of theories around why the incidence has gone up during COVID-19. Most of these are just theories with no evidence. What we do know for sure is COVID-19 disrupts our immune system, and more severe the disease higher is the chance of mucormycosis. Similarly, higher the level of blood sugar, higher is the chance of this fungal infection. So, if you are infected with COVID-19 make sure your blood sugar is under control and you ensure the disease doesn’t become severe. In worst case scenario, if infection does occur and Amphotericin B is not available, maybe Posoconazole + Deferasirox might work.
Finally- I would like to highlight here once again- the steps that I took to treat my family were unique and were forced due to the extreme constraints I was facing. Also, I am a trained registered doctor with a valid license to practice allopathy. My humble request is PLEASE DO NOT TAKE ANY MEDICINE OR FOLLOW ANY LINE OF TREATMENT WITHOUT CONSULTING YOUR PHYSICIAN.
References
[49] “Scorched Earth.” https://spartacus-educational.com/RUSearth.htm (accessed Jun. 04, 2021).



Thank you Dr Subir for sharing this interesting review. I totally agree with your experience as I managed my family and friends on nearly similar lines (till day. 14! – after that time I became lax!!).
I have a question as to which oral corticosteroid was used by you.
I have a strange personal experience (and some published literature) of getter better outcomes with Dexamethasone as compared to Methylprednisolone though both have identical modes of action with differences only in their PK profile.
Do you think this is possible.
I use prednisolone. I don’t see much difference between methylprednisolone and prednisolone considering the short duration of use. However, I personally feel prednisolone is quicker to act and its action vanishes off quickly compared to dexamethasone.
There is noticeably a bundle to know about this. I assume you made certain nice points in features also.
I am glad that you found this post useful!
I agree with your point of view, your article has given me a lot of help and benefited me a lot. Thanks. Hope you continue to write such excellent articles.
This was beautiful Admin. Thank you for your reflections.
I am truly thankful to the owner of this web site who has shared this fantastic piece of writing at at this place.
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
Cool that really helps, thank you.
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
Pretty! This has been a really wonderful post. Many thanks for providing these details.
I think this post makes sense and really helps me, so far I’m still confused, after reading the posts on this website I understand.
Cool that really helps, thank you.
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
There is definately a lot to find out about this subject. I like all the points you made
I just like the helpful information you provide in your articles
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
Cool that really helps, thank you.
very informative articles or reviews at this time.
Pretty! This has been a really wonderful post. Many thanks for providing these details.
Cool that really helps, thank you.
Cool that really helps, thank you.
Thanks for shening. I read many of your blog posts, cool, your blog is very good.
Try to slowly read the articles on this website, don’t just comment, I think the posts on this page are very helpful, because I understand the intent of the author of this article.
Thanks for a marvelous posting! I genuinely enjoyed reading it, you are a great author.I will always bookmark your blog and will often come back down the road. I want to encourage continue your great job, have a nice weekend!
Hi! I’m at work surfing around your blog from my new iphone 4! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the fantastic work!
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
Its such as you learn my thoughts! You seem to grasp a
lot approximately this, such as you wrote the book in it or something.
I think that you just can do with some p.c.
to force the message house a little bit, but other than that, this is excellent blog.
A fantastic read. I will certainly be back.
Having read this I believed it was very enlightening. I appreciate you finding the
time and effort to put this content together. I once again find myself
personally spending way too much time both reading and posting comments.
But so what, it was still worth it!
Wonderful beat ! I would like to apprentice whilst you amend your website, how can i subscribe for a weblog website?
The account aided me a acceptable deal. I had been tiny bit acquainted of this your broadcast provided bright transparent
idea
This is a topic that is close to my heart…
Many thanks! Exactly where are your contact details though?
Hi! I’m at work surfing around your blog from my new iphone 4! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the fantastic work!
Cool that really helps, thank you.
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
I just like the helpful information you provide in your articles
I appreciate you sharing this blog post. Thanks Again. Cool.
Really enjoyed this blog. Fantastic.
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
I don’t commonly comment but I gotta tell thankyou for the post on this perfect one : D.
This was beautiful Admin. Thank you for your reflections.
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
Great information shared.. really enjoyed reading this post thank you author for sharing this post .. appreciated
You have noted very interesting points! ps decent web site. “Formal education will make you a living self-education will make you a fortune.” by Jim Rohn.
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post
I have not checked in here for some time since I thought it was getting boring, but the last few posts are great quality so I guess I’ll add you back to my daily bloglist. You deserve it my friend 🙂
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
I appreciate you sharing this blog post. Thanks Again. Cool.
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
Yeah bookmaking this wasn’t a risky decision outstanding post!.
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
I need to to thank you for this fantastic read!! I definitely loved every bit of it. I have you bookmarked to check out new stuff you post?
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
This was beautiful Admin. Thank you for your reflections.
I think the content you share is interesting, but for me there is still something missing, because the things discussed above are not important to talk about today.
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
I carry on listening to the reports speak about getting free online grant applications so I have been looking around for the most excellent site to get one. Could you advise me please, where could i get some?
I gotta favorite this web site it seems very helpful invaluable
I’m often to blogging and i really appreciate your content. The article has actually peaks my interest. I’m going to bookmark your web site and maintain checking for brand spanking new information.
Great information shared.. really enjoyed reading this post thank you author for sharing this post .. appreciated
Good write-up, I am normal visitor of one’s site, maintain up the nice operate, and It’s going to be a regular visitor for a lengthy time.
There is definately a lot to find out about this subject. I like all the points you made
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
Nice post. I learn something totally new and challenging on websites
Thanks for a marvelous posting! I genuinely enjoyed reading it, you are a great author.I will always bookmark your blog and will often come back down the road. I want to encourage continue your great job, have a nice weekend!
Cool that really helps, thank you.
I appreciate you sharing this blog post. Thanks Again. Cool.