Table of Contents
Key Take-aways from This Article:
- Platelet transfusion is harmful in children if the platelets belong to adult donors
- Platelets from biologically aged donors can have deleterious effects, if transfused to any adult patient.
- Platelets hold memory of inflammatory insults as a child grows and becomes an adult.
- One easy way to avoid such complications is to use platelets only from those donors whose CD4:CD8 ratio is <1 and >2.5.
Issue With Platelet Transfusion in Children
Platelet transfusion is a procedure where platelets from a donor are given to a patient who has low platelet count or bleeding problems. This can be done to treat or prevent bleeding due to various causes, such as trauma, surgery, cancer or blood disorders.
Clinicians have noted that lower platelet count in children is associated with significant risk of bleeding and mortality.(1) Plasma and platelet transfusions are frequently administered to critically ill children to prevent bleeding and help treat active bleeding. In 2015, the American Association of Blood Banks (AABB) National Blood Collection and Utilization Surveys noted that 48,000 children received 165,000 apheresis platelet units and 29,000 children received 74,000 plasma units. (2)
Unfortunately, platelet transfusion in children often leads to worse clinical outcomes. (3) Children who receive platelet transfusion have higher odds of dying versus those who Do NOT receive platelet transfusion (except where disease is extremely severe).(4)
When I used to practice, I too had a similar observation. For a very long time, I was troubled by this paradox with no answer. Then, few weeks back I was in Montreal attending ISTH-2023. International Society on Thrombosis and Haemostasis (ISTH) Congress is one of largest international conference where global experts in the space of hematology come together and deliberate on latest science in thrombosis and hemostasis. On Tuesday morning (27 Jan 2023), Dr Craig Morrel from the University of Rochester presented his findings on his research with platelets. And it was in this session that I found the answer to this decade long mystery on why platelet transfusion was dangerous for children.
Dr Morrel’s data shed light on an intriguing phenomenon: platelets from adults differ from those of children. In his talk, Dr Morrel explained how platelets possess memory of inflammatory insults experienced during one’s journey from childhood to adulthood, and how this mechanism makes it dangerous when adult platelets are transfused to children.
Armed with these insights, I started researching further and eventually ended up writing this article.
Aging Transforms Platelets
Platelets are small, disc-shaped cells that circulate in the blood and help stop bleeding by forming clots. Although not appreciated by many, platelets are critical components of our immune system. Our immune system consists of defensive responses that aim to counter infections, injuries or other harmful stimuli. These defensive responses lead to inflammation. Inflammation can be imagined as a biological flame. While this flame is directed to destroy the harmful invaders and repair damage, sometimes the same flame of inflammation can become chronic or excessive, leading to tissue damage and diseases.
Since platelets are integral components of our immune system, they are actively involved in the process of inflammation. They actively participate in the inflammatory process by releasing various substances that can modify the responses of other cells, such as white blood cells and endothelial cells (the cells that line the blood vessels).
One of the key principles of an effective defense system is to ensure memory of your past interactions with enemies. Research now shows that platelets have the capacity to remember such interactions. Recent studies have shown that platelets can exhibit a memory-like response to repeated inflammatory stimuli. Hence, platelets that have been exposed to inflammation before can react differently when they encounter the same or similar stimuli again. For example, they can become more or less activated, secrete more or less substances, or change their shape or surface receptors. It’s as if platelets hold a personal diary of their encounters, enabling them to adapt and protect the body with enhanced precision. (5)
This memory-like response in platelets is thought to be mediated by epigenetic mechanisms, which are changes in gene expression that do not involve changes in DNA sequence. Epigenetic mechanisms can affect how genes are turned on or off by modifying the DNA or the proteins that wrap around it.
One way to understand how this works is by imagining that a platelet is a cook and has a recipe book. Depending on previous experiences, some pages of the recipe book get torn or folded or copied. Some words can get erased, some sentences can get jittered. Such changes would completely change what food items this platelet can now prepare and how those food items would taste.
This memory-based response in platelets can have implications for their functions in health and disease. For instance, it can affect their ability to form clots, adhere to blood vessels, diffuse into tissues, or interact with other cells. It can also affect their role in immunity and inflammation, such as modulating the activation and recruitment of white blood cells, enhancing or suppressing the inflammatory response, or influencing the resolution of inflammation.
The most important take-away here is that aging introduces individual specific changes. Younger the platelets are, more favorable would be the outcome when transfused to a patient in need.
Platelet Transfusion in Children Is Risky
Platelet transfusion is a common practice in medicine, especially for patients who have low platelet count or bleeding problems. As noted earlier, platelet transfusion is not without risks or complications. One of the potential problems is the compatibility between the donor and the recipient platelets. This can be affected by various factors. One of the factors that may affect platelet compatibility is the age of the donor and the recipient. Studies have shown that platelets from adults differ from those from children in several aspects, such as size, shape, density, metabolism, activation status, gene expression and function. These differences may reflect the different developmental stages and environmental exposures of adults and children. (6)
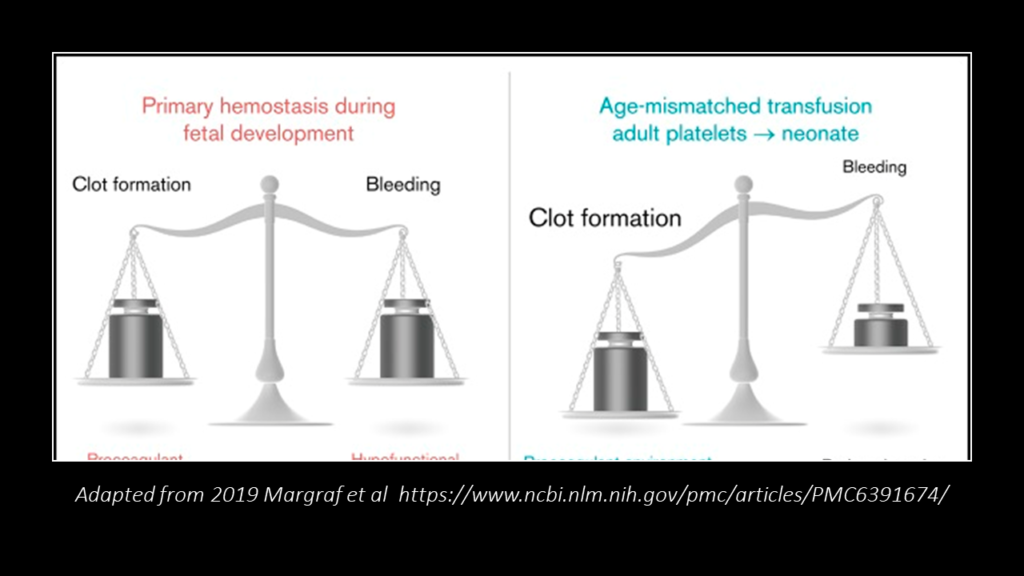
But the most important difference between platelets of children and adults is in the amount of inflammation exposure. This means that platelets from adults may have been exposed to more inflammation than those from children, and thus may have different epigenetic profiles and functions. As discussed above, platelets can hold memory of inflammatory insults as a child grows and becomes an adult. This mismatch in the level of “inflammatory” memories has significant consequences when platelets are transfused from adults to children. (7)
For example, if platelets from adults have been primed by inflammation to become more activated or pro-inflammatory, they may cause adverse effects when transfused to children who have less inflammatory exposure or tolerance. Conversely, if platelets from adults have been primed by inflammation to become less activated or anti-inflammatory, they may impair the immune response or wound healing when transfused to children who need more inflammatory support. This explains why Dr Morrel’s data showed platelet transfusion from adults to children might be risky.
To illustrate the implications, let’s imagine platelets as liquid cement that hasn’t hardened. If this cement level is low, it won’t be able to plug all the cracks adequately. The only way to address this situation is to add more liquid cement. If you add hardened cement, it won’t work. It will- in fact- create more issues. The liquid cement here represents the platelets in a young kid. The hard cement represents platelets from an adult- molded and hardened by inflammation faced by that adult during his/her lifetime. Rather than being therapeutic, such mismatch can create chaos and destruction. This is why platelet transfusion from adults have worse outcomes in children.
While the entire discussion has been referring to platelet transfusion, the same conclusions would hold true for even plasma transfusion or blood transfusion.
Can Platelet Transfusion Be Risky in Adults Too?
What about adults who need platelet transfusion? Won’t there be a similar issue?
Well, these are the right questions one must ponder upon whenever we think of platelet transfusion or even blood transfusion. Imagine Sam- a 40 years old male who lived in a very clean and protected environment all his life. One day, Sam goes to Sri Lanka where he contracts Dengue. His platelets drops down critically and now his doctors decide that Sam must be transfused with platelets. What if he receives platelets that came from someone who was diabetic and hypertensive and had multiple infections and hospitalizations? Sam’s platelets don’t have as much “inflammatory” memory as the platelets he is getting transfused with.
Based on current research and insights that I have, I definitely believe that such platelet transfusion would do more harm to Sam.
How to Tackle This Issue?
Theoretically, one strategy involves utilizing platelets from donors who are closer in age to the recipient in need. These platelets might share similar experiences and memories, allowing for a more compatible and effective response.
But, in practice, this strategy would fail on two counts. First, it would be exceedingly difficult to find a platelet donor who would match the patient’s age, in case the patient is very young. The other aspect is that chronological age hardly is measure of total inflammation etched in the memory of platelets. This “total inflammation” is actually what defines biological age. A 50 year old healthy male with no chronic diseases might be biologically younger than a 20 year old male suffering from rheumatoid arthritis and diabetes.
One efficient way to handle this issue to measure biological age. Do not use platelets from any donor who has biologically aged significantly. Then, the next question is- how would you measure biological age. There are various ways. But my favorite way is to use CD4:CD8 ratio. It’s not perfect. But it’s easy and straightforward. Do not use platelets or blood from donors whose CD4:CD8 ratio is <1 and >2.5.
If you want to learn more about why I love CD4:CD8 ratio, please read my article on this HERE.
Concluding remarks
Platelets are small but important cells that play extremely important roles in immunity and inflammation. Studies now show that platelets hold memory of inflammatory insults as a child grows and becomes an adult. These memories shape platelets specifically to cater to the biological needs of that specific individual. Hence, platelets from adults can lead to unfavorable outcomes, if transfused to a young patient. Similar outcomes might occur in adult patients as well, if biologically aged platelets are transfused.
One easy way to avoid such complications is to use platelets only from those donors whose CD4:CD8 ratio is <1 and >2.5.




Thanks a lot for the post.Really looking forward to read more. Awesome.
Fantastic blog. Keep writing.
Bravo, what phrase…, an excellent idea
You are a very clever individual!
Usually I do not read article on blogs however I would like to say that this writeup very compelled me to take a look at and do it Your writing style has been amazed me Thank you very nice article
Its like you read my mind You appear to know a lot about this like you wrote the book in it or something I think that you could do with some pics to drive the message home a little bit but instead of that this is fantastic blog An excellent read I will certainly be back
Hello.This article was extremely fascinating, particularly because I was investigating for thoughts on this subject last Monday.
I genuinely value your work, Great post.
Terrific work! This is the type of info that should be shared around the web. Shame on the search engines for not positioning this post higher! Come on over and visit my site . Thanks =)