Table of Contents
Introduction
“Who will require hospitalization in COVID-19?”
“Is there a simple number that can be used to identify which of the COVID-19 infected patients will develop complications and will require additional support?“
A recently conducted survey shows that this is a burning issue in today’s pandemic haunting everyone.
It’s clear that COVID-19 infection can’t be really stopped. One wave after the other have been raging across the world and will continue. Millions have died. It’s really terrifying. But we also know that majority recover easily. Only a few require hospitalization. Despite this fact, each wave of this pandemic overloads the existing healthcare systems with hospitals running out of beds.
At present there is really no way to predict right at the start which patient, infected with COVID-19, will develop complications. If such prediction is made possible, we shall be able to focus our resources on only those who really need, and decisively intervene at a very early stage- while other patients might just relax at their homes. Such early intervention, focused on the ones who will eventually develop complications on COVID-19 infection, will significantly reduce hospitalization rate and mortality. But is there a way to accurately predict which patient will deteriorate and will require such early intervention?
This is exactly what we will try to answer. Let’s see if we succeed.

This post is the second part of the four-parts series that intends to eventually show how we can easily predict outcomes of COVID-19 infected patient at a very early stage. (If you haven’t read the first part, click HERE).
(I would have loved to cover the entire thing in just one single post. But, its really important for the reader to understand the fundamentals of virology and immunology involved. And I will be covering those in a very simple layman language. And a single post covering all these aspects will easily cross 20,000 words- nearly a book in itself!)
What will we learn in this post?
In the first part of this series we focused on understanding why it is more important to predict who will die in COVID-19 rather than just focusing on prevention and treatment of all. We also explored how vaccines and anti- viral drugs might not help in completely wiping off this pandemic.
In this post we will explore in detail what really happens “COVID-19 induced cytokine storm” and how do we go about controlling the same. It is this entity of cytokine storm that is the real reason why few infected patients land up in hospitals and get killed. We will explore this complicated topic is a very simple language such that every reader, irrespective of his/her background will easily understand how COVID-19 has been killing millions.
The Storm of Destruction- Understanding cytokine storm in COVID-19 infection
Life is a Battle- Field

In the realm of living world, only few organisms don’t kill others to survive. Only photosynthetic plants and chemoautotrophic bacteria don’t need to invade other living species for generating energy. However, excluding these autotrophs, all other biological living systems resemble the game of chess.
Each such “non- autotrophic” organism- whether it’s simple unicellular structure like a virus or a bacterium, or a complex multicellular organism such as a human- is always in a constant struggle of protecting its own camp of life and attacking other lives’ camps. Survival is dependent equally on both aspects of this struggle. If it cannot attack and plunder another living organism, it will die hungry with no energy to fuel its life. If it cannot defend itself from attack from another living organism, of course it will cease to exist.
Principles of Defense
For any living organism, an accurate defense works on few principles[1] [2]
- It should be able to first differentiate between which particles/component are “own” and which are “foreign”. These particles/components are also known as antigens. Each antigen has set of signatures known as epitopes.
- There has to be a constant surveillance to identify, categorize and monitor foreign antigens.
- Body should be able to respond immediately to a foreign antigen and eliminate possible any form of threat
- For those antigens which don’t bow down to immediate response, must be dealt with specific and more effective responses
- Every successful response must be recorded and remembered so that next time when same threat attacks, specific response is faster
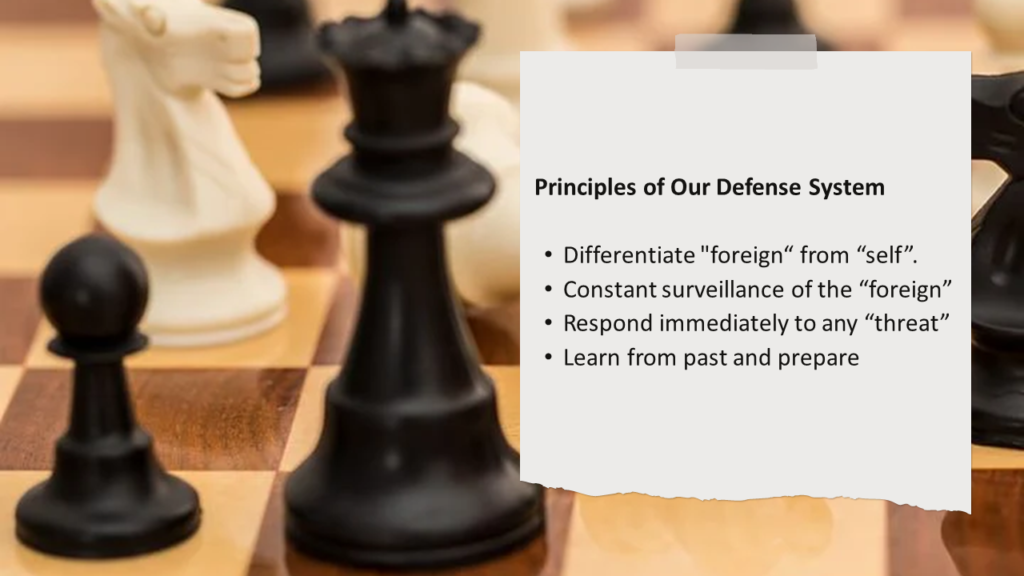
Based on these principles, complex organisms with thousands of years of evolution have developed a very sophisticated defense systems (also known as immune systems) that allow seamless survival and propagation of their respective species.
Self vs Foreign
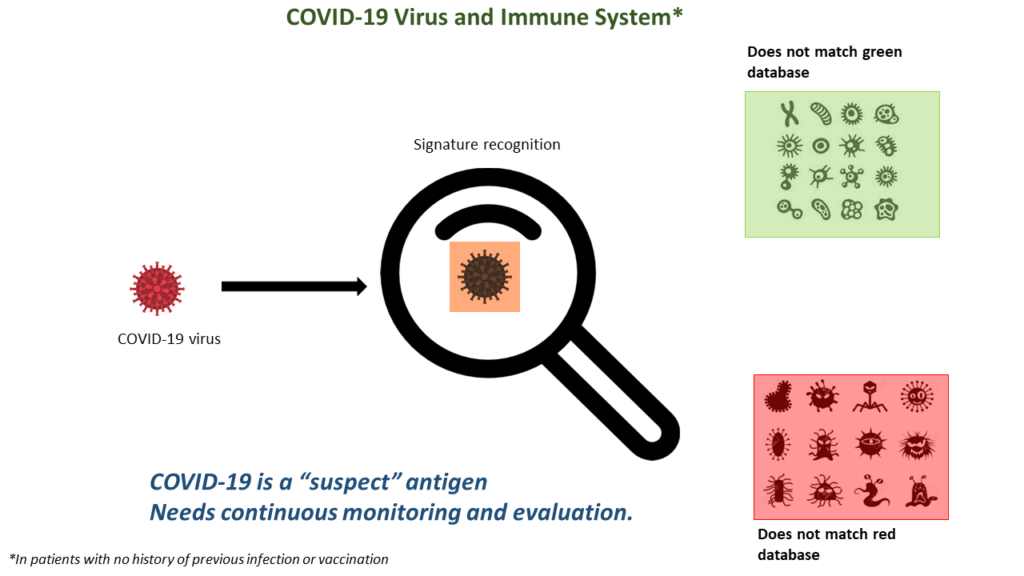
Our human immune system has the innate ability to distinguish between what is its own and what is foreign. This ability is important so that the body’s defense system can defend against any foreign threats such as deadly viruses or bacteria, while making sure that it does not attack and kill its own cells. The way this system works is via signature and pattern recognition. Each organic particle in our body can be called as an antigen. And each antigen bears a set of signatures called epitopes. Our defense system maintains two databases of such signatures- one can be called “green database” and other can be called “red database”.
Any antigen that has signatures matching the “green database” is recognized as harmless and is not attacked. Any antigen whose signatures match the any of the ones in the “red database” is identified as dangerous- such antigens will be attacked and destroyed. Any other antigen, whose signatures do not match the “green database” and nor is part of the “red database” can be called as a “suspect”.

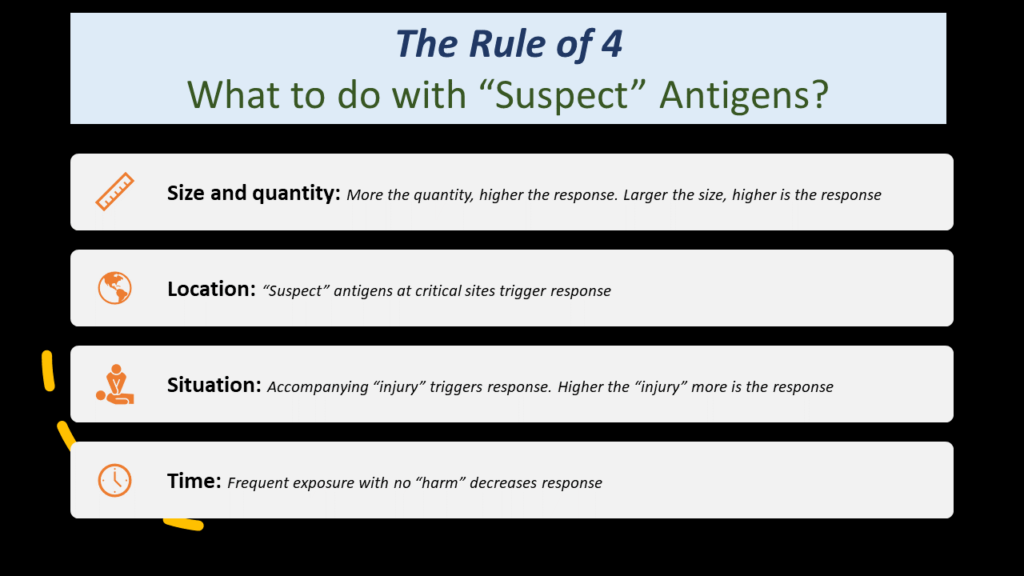
For such “suspect” antigens, the defense response depends of size, amount, location and level of damage caused by the uncategorized “suspect” antigen. To be on the safer side of the error, our defense system follows 4 simple rules of thumb.
Rule 1: SIZE & QUANTITY– larger the size, stronger would be the response. So, larger the size of the “suspect” antigen, greater will be the defense response, although in reality this particle might not be causing any harm on its own. So is true in terms of quantity- more the quantity of the “suspect” antigen particles, greater will be the defense response, although in reality this particle might be absolutely harmless.
Rule 2: LOCATION– “suspect” antigens located at certain zones will invite severe defense response compared to other zones. More critical and improbable the location of the “suspect” antigens, more accentuated will the defense response against such antigens. For example, airways and gut are generally tolerant and reactions are pretty much contained against antigens. However, if the same antigen is found in critical organs such as brain etc., body’s defense will not tolerate, and a gruesome attack will be launched.
Rule 3: SITUATION– small “suspect” antigens entering harmlessly will not be seen with much interest by our immune system. But entry of same antigens in the same location with some accompanying damage can provoke immune system to mount attack on these particles. This principle is utilized greatly while developing vaccines. A vaccine can be bound to a particle called “adjuvant” which causes some amount of inflammation. This causes immune system to quickly get activated by the vaccine, thus improving efficacy of the vaccine. Hence the painful cellular DPT vaccine (for Diphtheria, Pertussis and Tetanus) is much more effective that the painless acellular DaPT vaccine.
Rule 4: TIME– a large “suspect” antigen might be dealt with furiously by our immune system on first contact. But if such contacts are frequent and actually not much damage is being recorded in association with this “suspect” antigen, immune system will learn to tolerate this antigen and eventually will record the structure of these epitopes into “green database”. This is how the concept of immune tolerance works. For example, one of the best ways of managing lactose intolerance is to reduce the quantity of lactose intake and slowly keep increasing the same over a period of time.
What is a virus?
A virus is a very interesting organism. Some biologists prefer calling a virus to be bordering between the definition of living and non- living things. A normal living cell is an enclosed organic box that has a book of instructions called genome and a set of machinery to read and execute these instructions.

A virus also is an enclosed organic box- but inside this box there is just the book and nothing else– there are no tools or mechanism intrinsically available for reading and executing the instructions coded that book. Without such capability of reading the genome (the book) and following the instructions, a virus alone is as good as any non-living organism. The only way a virus can be brought to life is by allowing someone else read and follow the instructions in the viral genome. This is what happens when a virus enters a host cell- the viral genome leaves its original organic box and enters the cell of the host. The host cell, with its fully functional genome reading tools, translates the viral genomic instructions [3]. In nature, the instructions coded in the viral genome are simple- they just code for how to make copies of the virus. Thus, the infected host cell starts making multiple copies of the virus. In some cases, this reading of viral genome is not immediate and for years can remain unread. This is what happens during the latent phase of Hepatitis B infection.
But in case of COVID-19 infection, this is fairly rapid.
COVID-19 vs Our Immune System
Once infected, the affected cells of the human respiratory tract will start reading the genome of COVID-19 without much delay and will start producing multiple copies of the virus. These virus particles will then start infecting other neighboring cells and these cells will also start make copies of the virus. Thus, a single COVID-19 virus particle potentially recruits our own cells to start producing millions of copies of COVID-19 [4].
Of course, immune system won’t remain quiet. COVID-19 viral antigens don’t match either the “green” or “red” databases. They are “suspects”. Hence, immune system then follows the 4 thumb rules discussed above. So, here is an antigen which is in a location that is not very critical and where foreign particles keep coming regularly. But the amount of antigen load is huge. So, in general, there will be some form of immediate immune response led by our innate immune system. It is exactly here where decisions made by the immune system will determine patient’s survival.
Interestingly, it is the excessive action rather than inaction of immune system that will be the cause of death in an unfortunate patient.
The Innate Immune System and COVID-19
Innate immune system is our primary line of defense and is immediate in its response to any threat. Seeing the huge number of “suspect” antigens, innate immune system gets activated. Local cells release defense chemicals known as “chemokines” which is akin to “call for help“. These chemokines attract defense cells such as neutrophils and lymphocytes to the site of infection. The capillary and lymphatic channels dilate so that the defense cells can flow in faster and in great numbers. The water in blood starts getting utilized to make mucous. Mucous is sticky and serves to imprison viral particles within its inherent mesh. Sensory nerves around bronchi and nose get activated- making the patient cough and sneeze. The mucous that has trapped thousands of viral particles get thrown out via coughing and sneezing. Its an innovative way of “washing out” the virus particles! The defense chemicals reach brain instructing it to go on “war” mode. In this mode, brain resets its thermostat to a higher level- body temperature rises leading to fever. Thousands of years of evolution have programmed our immune to system to the fact that invaders efficiently invade only when temperature is conducive. Fever is a defense as a part of that evolutionary programming- higher temperature tends to inactivate the invaders. [5]
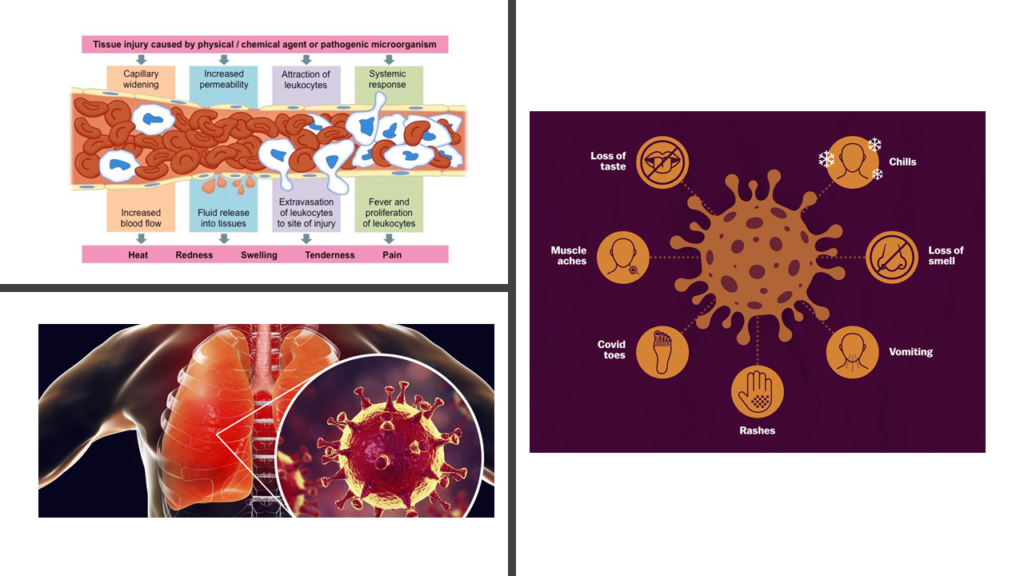
Neutrophils, lymphocytes, vasodilation, sneezing, coughing, fever- these are generalized immune response driven by our innate immune system to immediately tackle the viral threat. The pattern of defense remains same irrespective of type of virus. In most cases, given enough time, this innate immune response is more than sufficient in tackling this threat by COVID-19. But our body doesn’t take any chances.
The Adaptive Immune System and COVID-19
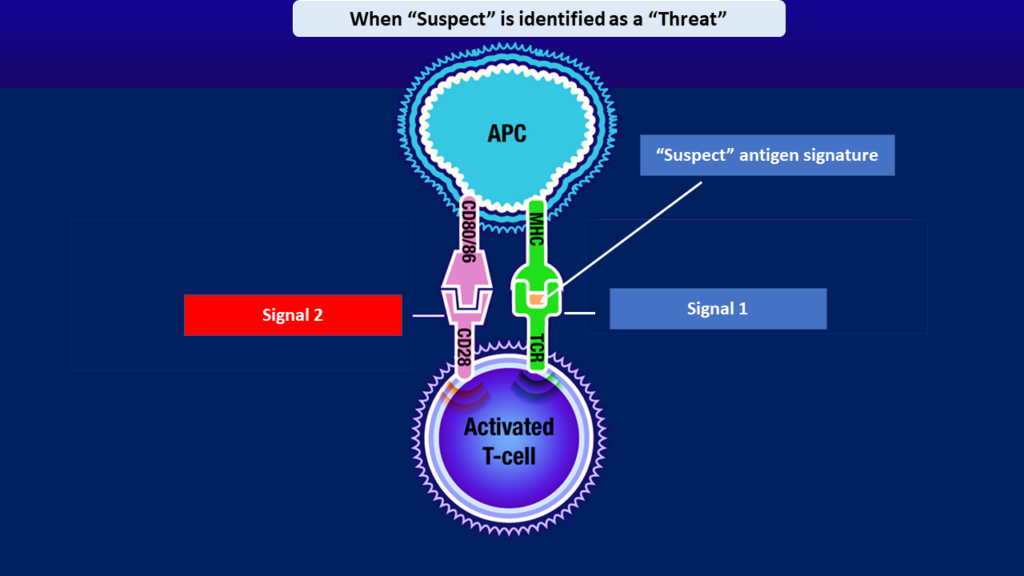
We have a set of “detective” cells whose job is to keep monitoring our body for any sort of “invasion”. These “detectives” are known as Antigen Presenting Cells (APCs)[6]. APCs act as bridge between innate and adaptive immune system. Adaptive immune system is the more mature elder brother of innate immune system. A foreign antigen detected by APCs alerts the adaptive immune system. If the signature of the foreign antigen matches the “green” database, adaptive system takes no action. If the signature of the foreign antigen matches the “red” database, adaptive system swings into immediate action and its response is specific against that antigen and this response is very powerful.
If any of the antigen signatures are part of “red” database, it just means that immune system had encountered that antigen earlier, had recognized it as dangerous and had learnt how to fight that danger. These learnings are stored in the memory of adaptive immune system. So, when the same “red” antigen attacks again, adaptive immune system knows from its memory exactly what to do.

However, when faced with a new antigen whose signatures don’t match either of the “green” or “red” databases, adaptive immune system is generally helpless initially. But this helplessness is not benign and should not be mistaken with uselessness. The adaptive immune system observes behavior of such antigens silently– its eyes and ears being the APCs. This observation is often called the “first signal”. Once threat is registered (based on the 4 thumb rules discussed above), APCs generate a “second signal”, also known as “co-stimulation”- this activates the adaptive immune system to enter the fight. It immediately starts analyzing the signatures of these “formerly suspect- now red” antigens, and starts preparing weapons that can target only those antigens with the pre- specified signatures. Such targeted biomolecules prepared by the adaptive immune system (such as antibodies, cytotoxic T cells etc) can locate the target signatures anywhere in the whole body and will destroy the antigens bearing those signatures [7].
In case of COVID-19 infection, along with the innate immunity, adaptive immunity too joins the battle- field. Targeted antibodies and specialized T cells locate the COVID-19 virus particles and destroy them.
The COVID-19 led “cytokine storm”
But, while battle is going on, collateral damage is expected. When a bomb explodes, enemy soldiers do get killed- but if there are civilians in that place, innocent lives get lost as well. In COVID-19, the battlefield lies in the lung parenchyma whose cells are essential for ensuring oxygen gets dissolved in blood and carbon- di- oxide gets eliminated. And in this battle, where innate immunity and adaptive immunity both are fighting with the virus particles, quite a large number of normal lung cells do get destroyed. Fighting viral infection is a bit different that fighting bacterial infections. In a bacterial infection, the invader is always (in most cases) outside the cell. You just need to target the invader and no one else. Of course, there will be some collateral damage due to immune attack- but it’s fairly limited in most cases because target is outside any cell.
In COVID-19 infection, you have 2 kinds of particles- ones who have infected the cell and are inside the cells and the other ones who are outside the cell, while on their way to infect other cells. To eliminate a virus lying “outside”, immune system will target the virus itself. But what about a COVID-19 virus inside a lung cell? No defense cells can enter our own cell to find and kill the virus. The only way out is to kill the “self” cell itself which is harboring the virus. So, if millions of lung cells harbor COVID-19 virus particles inside, immune system might end up killing all these lung cells. And our immune system is programmed to identify any “dead self- cells” as threats. Once you have killed enough of your own cells, the “threat antigens” from the viruses and the dead self- cells go on to trigger a vicious cycle that will lead to more killing of self-cells. At the end, you get what is known as cytokine storm which will end up resulting in pulmonary failure.
This is a very simplistic picture of what really goes on in a “cytokine storm”[8]- large amount of chemicals known as cytokines are released when our own cells die “crying for help“. When the number self- cells dying is significant, body’s immune system feels it’s under attack, and it unleashes itself with more force. But unfortunately, this “more” force explodes amongst the lung cells again killing large number of these lung cells. And the cycle keeps continuing, feeding upon itself and growing. Most often than not, in this situation, patient will die.
Combating the storm:
(Note: DO NOT try any therapy discussed here unless prescribed by a registered medical practitioner)
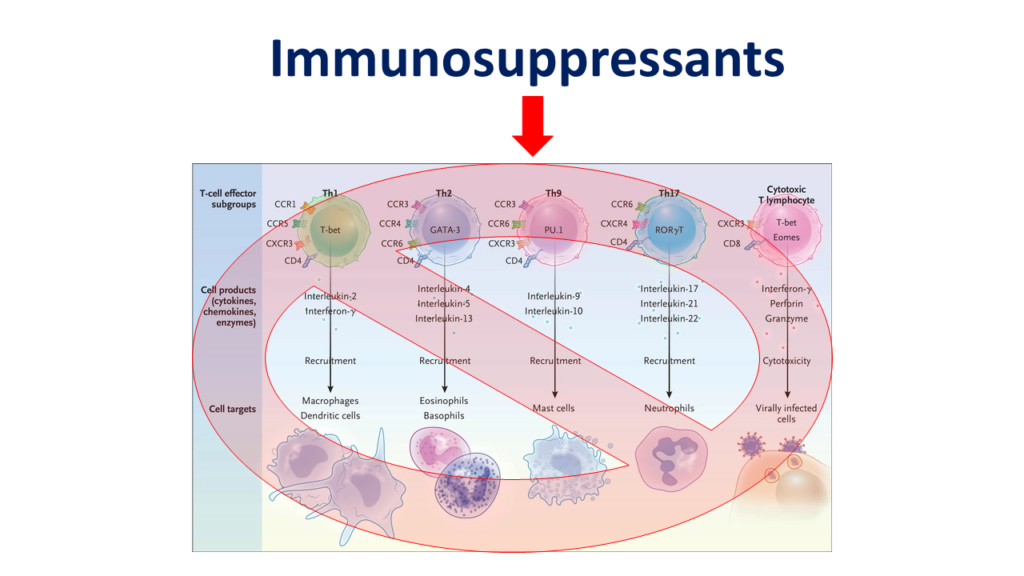
Corticosteroids, Tocilizumab
Cytokine storm is an outcome of relentless attack by our immune system, where immune system has gone mad and is blindly unleashing all its weapons. This is where the idea of using immunomodulators and immunosuppressants feature. IL-6, TNF alfa etc [9] are very important chemicals (they are also called cytokines) that act as fuel to the fire of cytokine storm. So, theoretically, IL-6 inhibitors like Tocilizumab or TNF alfa inhibitors like Infliximab (which are already commercially available) can break the chain of self-propagating cytokine storm. But the results, when used in critically ill COVID-19 patients, have not been extremely encouraging though. Tocilizumab doesn’t work in all patients. There are two important reasons for this. IL-6, TNF- alfa are not the only cytokines and depending on individual genetics one cytokine might be more dominant than other. And hence, in a recent study, Tocilizumab failed to provide any benefit to patients hospitalized with moderately severe COVID-19 infection [12].
What seems to be working is liberal use of generalized immunosuppressants such as corticosteroids. Concentrated use of corticosteroids will universally dampen activity of all immune cells and hence might be the most effective strategy to prevent or stop cytokine storm. And this life- saving use of corticosteroids have been proven in several high-quality clinical studies [10].
(Having said that, there still will be few patients who won’t respond to even very high doses of corticosteroids and, in these exceptional patients immunomodulators like Tocilizumab or Tofacitinib might work.)
About Hydroxychloroquine
Theoretically, in early cases if immune system is dampened, no cytokine storm should happen. This was the logic that soared hopes on early use of Hydroxychloroquine (HCQ)[11]. But, in clinical studies, these hopes did not materialize as expected. Of course, one reason might be data manipulation since HCQ is very cheap, and big pharmaceutical companies making antivirals would stand to lose the chance of earning in billions. But data can’t be fudged in all studies, and in general the results were mixed. Technically speaking, it was more of a desperation rather than science to put hopes on success of universal use of HCQ. If you use HCQ in a patient with mild infection in early stages, you will make patient’s immune system weak. But it is the same immune system that will allow elimination of all the viral particles in most patients without causing any cytokine storm. If such immune system is weakened with HCQ, you will have virus replicating more rapidly and not getting eliminated. The “suspect” antigen load will keep rising. And we need to remember that HCQ is quite a weak immunomodulator compared to others. Beyond a certain point the viral antigen load will be high enough to eventually trigger immune system. Eventually such immune system will break the shackles of HCQ and unleash heavily to tackle the antigens. But by that time the amount of antigens load would be so high, with so many cells infected, that immune system will end attacking much higher number of normal cells, potentially triggering cytokine storm. So, in theory, you might have caused cytokine storm by introducing HCQ early.
Based on the available knowledge of how COVID-19 attacks and how HCQ works, it’s almost hilarious to try understanding the logic behind studies assessing efficacy of HCQ as prophylaxis to prevent COVID-19. One logic can be some initial laboratory studies suggesting antiviral properties of HCQ on coronaviruses. But if this is the reasoning, then isn’t it better to test documented strong antivirals such Remdesivir or Favipiravir rather than HCQ for prophylaxis? One has to be, although, aware that rampant use of antivirals can backfire- it will only drive development of COVID-19 mutants resistant to antivirals.
Role of antivirals, convalescent plasma etc in combating cytokine storm
Antivirals- Remdesivir, Favipiravir
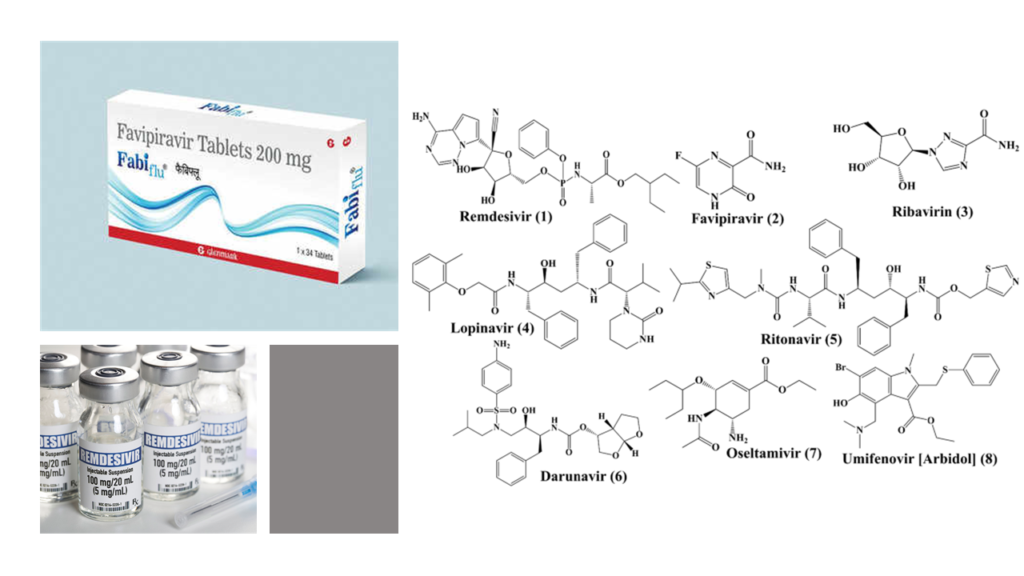
Antivirals such as Remdesivir and Favipiravir serve to reduce to the antigen load by halting viral replication. But, issue is, once the cytokine storm starts, one of the critical factors that keep giving fuel to the engulfing fire is the ever- increasing antigen load from the dead “self- cells”. As the fire spreads, more and more “self- cells” die adding further fuel. It’s no longer just the virus. Hence the role in controlling cytokine storm seems controversial. And this has been seen in clinical studies as well. In hospitalized COVID-19 patients powerful antivirals like Remdesivir haven’t shown any benefit in improving survival [13]. I personally feel that these antivirals can have a beneficial role when introduced early in the disease course, when the infection is mild. By decreasing the viral load, chances are, the antivirals might help in decreasing the chances of patient progressing into cytokine storm. But, we need a good clinical trial to validate this hypothesis.
Convalescent Plasma
Blood consists of cells floating in a fluid rich in chemicals important for sustaining life. If you remove these cells from blood, what is left behind is known as plasma. When our body is attacked by COVID-19 virus, our defense cells prepare and unleash several weapons. One such weapon is known as “antibodies” (also known as immunoglobulins– abbreviated as Ig). These immunoglobulins can be of 5 different types (IgG, IgA, IgM, IgD and IgE). IgG is highly specific and can easily destroy the target virus. So, as far as theory goes, patients who have recovered from COVID-19 must have powerful IgGs in their blood which can neutralize the virus. If so, then it can be a great idea to collect plasma from such a patient who has recovered from COVID-19. Plasma collected from such recovered patient is known as convalescent plasma. This convalescent plasma can then be used to treat any other patient currently suffering from COVID-19; the anti- COVID IgGs in this convalescent plasma is expected to destroy COVID-19 virus particles in a patient with active infection.
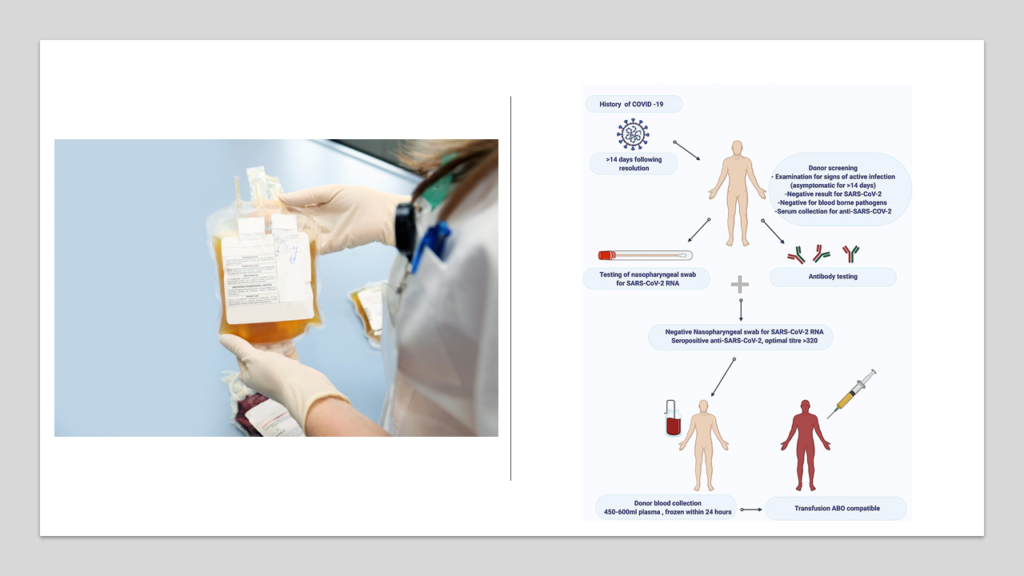
Unfortunately convalescent plasma hasn’t been shown to be as effective as was expected. Several studies focusing on use of convalescent plasma in patients with COVID-19 who had moderate to severe illness failed to show significant clinical benefit [14].
To understand this mismatch between expected benefits of convalescent plasma and actual results, you need to understand how antibodies work. Antibodies are few amongst the several weapons prepared by our adaptive immune system. They are very powerful and highly specific. Unfortunately they are designed to tackle “threats” roaming outside the cell. Once the “threat” enters a cell, antibodies won’t really work, they cannot enter the cell. And viruses are primarily intracellular. Its only when the want to infect another cell, they have come out. In early stages of infection, fewer cells are infected. This is when convalescent plasma should really be useful. Used early, convalescent plasma will kill any virus coming out of these cells and prevent other cells from getting infected. This should prevent progression into cytokine storm.
But during COVID-19 induced cytokine storm, as I have discussed earlier, one of the critical factors that keeps giving fuel to the engulfing fire is the ever- increasing antigen load from the dead “self- cells”. As the fire spreads, more and more “self- cells” die adding further fuel. It’s no longer just the virus. And hence, convalescent plasma might NOT work if used when cytokine storm is in full force.
Others
With most of the treatment regimens failing in severe cases of COVID-19, government is literally approving any therapy that shows some theoretical promise. Recently, experimental therapies such as interferons (launched in India by Zydus Cadila, under the brand name “VIRAFIN“) and Itolizumab (launched in India by Biocon, under the brand name “ALZUMAB“) have been approved in India. Unfortunately there is no convincing evidence to show they are effective in COVID-19 patients. Data from the SOLIDARITY study is clear- interferon regimens had little or no effect on hospitalized patients with Covid-19 [15]. There are few studies that have evaluated role of Itolizumab. Issue is that the studies are too few and each study is with extremely small number of patients. Directionally, it looks like Itolizumab might be as effective (or ineffective) as Tocilizumab- but it’s too early to conclude anything.
Let me end this part by saying that each individual is different. While some drugs might work, some might not work. In some, cytokine storm might be dominated by IL-6. In them Tocilizumab might work. In few, it might be let’s say TNF alfa driven. Maybe in such patients biologics such as Infliximab or Adalimumab can work. In few patients, the whole storm might be antibodies dominated. In these cases, maybe Rituximab might work.
Drugs like corticosteroids dampen nearly all cells and chemicals of immune system. Hence, most often, they work in all segments of patients. If so, then even JAK inhibitors such as Tofacitinib (XELJANZ, by Pfizer) might work as well. This action of Tofacitinib has already been proven in a recent study- Tofacitinib might be able save lives by effectively curbing COVID-19 cytokine storm [16]. There has been similar anecdotal experiences in India as well.
I want to quote one personal experience here. I know of a patient who worsened into severe cytokine storm due to COVID-19. The patient was on ventilator. High dose of steroids were being given to this patient intravenously (500 mg methyl- prednisolone per day). 3 days into this heavy steroid dosing and still SpO2 was barely touching 70%, despite the patient being on ventilator. Inflammatory markers like CRP, D-Dimers, Ferritin, LDH were just continually rising. This patient was amongst those few unfortunate exceptions who don’t respond to steroids. Adding to this issue was another unfortunate situation that Tocilizumab was not available and couldn’t be procured. There was no hope- it was assumed that this patient will not survive. But the attending physician did not give up. After lot of brainstorming, he figured out that he can try either Etanercept or Tofacitinib (since both are potent immunomodulators just like Tocilizumab, and, more importantly, both were available). Finally, he went ahead with Tofacitinib as a desperate last resort. And then literally miracle happened. Within 24 hours, all the inflammatory markers started dropping rapidly. SpO2, which was earlier refusing to rise beyond 80%, was now suddenly touching 100% consistently. The cytokine storm was gone! Tofacitinib literally snatched the patient out of the jaws of death. Of course one cannot use generalize this experience- but is worth an attempt in terminal COVID-19 infected patients not responding to anything.
(The thought of exploring Tofacitinib in this post came to me after a long discussion with Dr Amit Hartalkar. Dr Hartalkar is a medical expert at Hartalkar Hospital, located in Chopda near Jalgaon– India. He is my senior from where I did my MBBS and has been successfully managing patients with COVID-19 cytokine storm. As it turned out, his suggestion regarding use of Tofacitinib has already been tested and proven in US by Dr Hayek and his team [16]. Further observations from experiences in India also suggested that Dr Hartalkar’s idea was bang on! )
We haven’t yet tested powerful immunosuppressants such as Basiliximab or anti- thymocyte globulin or tacrolimus which are routinely used in organ transplantation. Maybe they will turn off the immune system and completely stop cytokine storm. But we don’t have these answers yet.
Also, what if turning off immune system itself kills the patient? We are surrounded by millions of dangerous pathogens- COVID is just one of them. You silence immune system to stop cytokine storm and you might end up with loads of other virus/bacteria/fungi rapidly and lethally attacking the patient.
These are all dangerous therapies- DO NOT try any therapy discussed here unless prescribed by a registered medical practitioner.
Can vaccines prevent cytokine storm?
I will start by giving the answer- vaccines definitely prevent cytokine storm.
We earlier saw that adaptive immune system, on facing a “confirmed threat” for the first time learns how to specifically combat the threat and stores these learnings. This specificity is key, and is important to ensure the response is purely against that specific threat with minimal collateral damage.
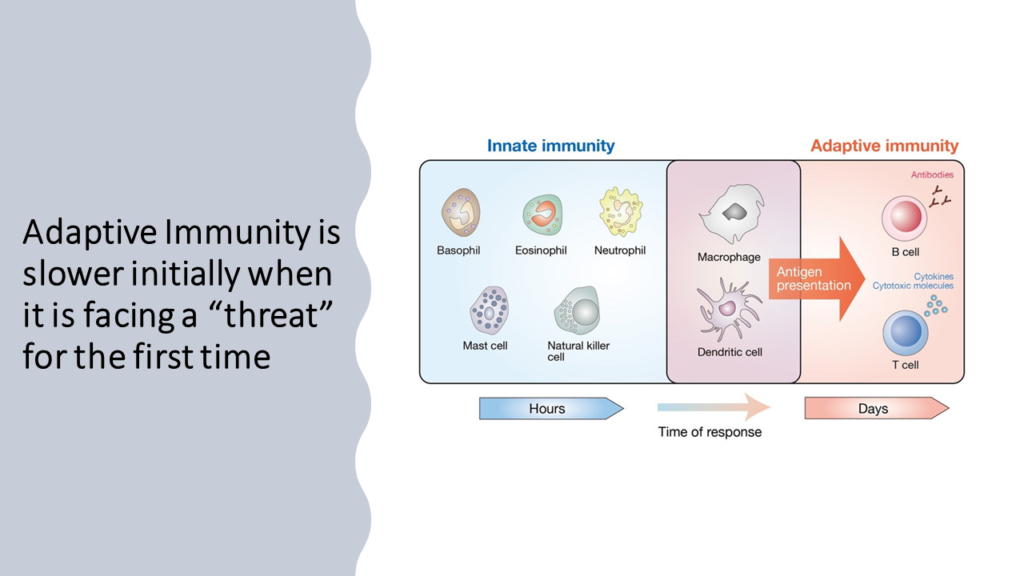
Next time, when the same threat comes adaptive immune system rapidly does exactly what’s needed to ward off the “threat” with very limited harm to “self- cells”.
Let’s use an analogy to visualize what’s really going on. When adaptive immune system faces a “confirmed threat” for the first time, it’s powerless at that exact moment (the fighting is done by innate immune system). But, it observes, gathers information and learns. This initial “learning journey” is known as primary response. The information collected and learnings gathered are used to set up a factory and production line to build weapons that will specifically kill the “threat” and no one else. Next time when the same threat attacks, adaptive immune system just collects the weapons from this factory specific to the treat and starts attacking the threat. This fast action by adaptive immune system on repeat exposure to a “threat” is known as secondary response.
(I have stolen this beautiful analogy of factory and production line from Dr Arindam Chakrabarty. He is my senior from where I did my MBBS and is currently working as Assistant Professor at SIU School of Medicine, Springfield, Illinois.)

Idea of vaccination is to just fool the adaptive immune system and make it believe that there is “threat”. In case of COVID-19 this is done via introducing “antigens” specific to COVID-19 virus. The vaccine is perfectly harmless and body is made to believe that the injected antigens are a threat. So, when vaccine is injected for the first time, adaptive immune system learns and generates primary response. Next time, when the real threat comes in the form of actual COVID-19 virus, the super- fast secondary response is initiated and adaptive immune system launches decisive attack on COVID-19. More the number of exposures to threats, better the body is prepared. Hence, vaccines are given in multiple shots at different time periods.
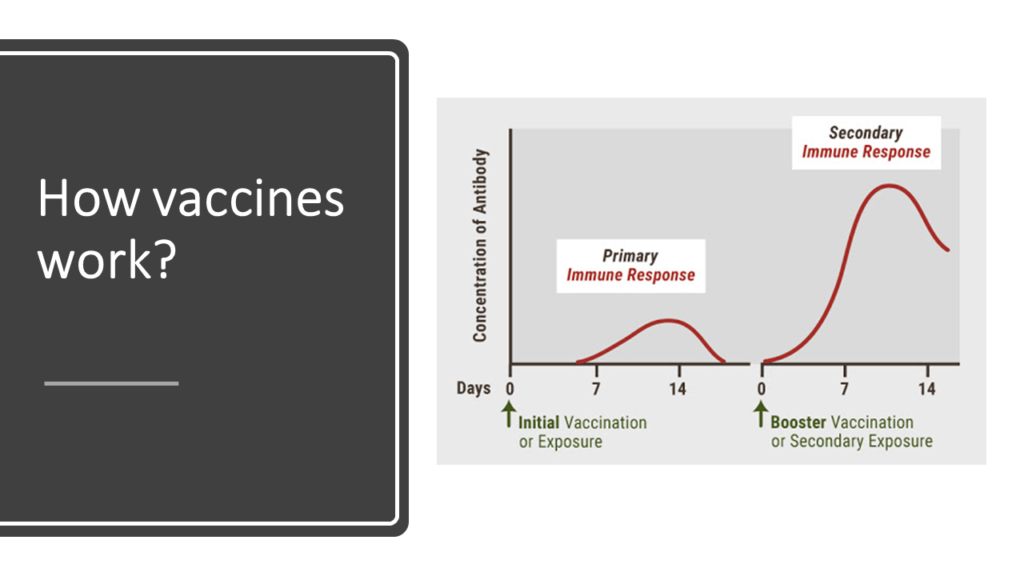
We just discussed that when adaptive immune system is exposed to a threat it has faced earlier, it rapidly generates secondary reaction that that does exactly what’s need to ward off the “threat” with very limited harm to “self- cells”. This “limited-harm-to-self-cells” property of secondary response is exactly what prevents cytokine storm. When COVID-19 virus enters a vaccinated person, adaptive immune system activates secondary immune response against the virus. This response is specific to the virus and does little damage to “self- cells” and prevents cytokine storm.

This post is not about vaccines. But I would like you to remember 3 critical things about COVID-19 vaccines:
- Take vaccines. They might not prevent infection in all, but will prevent COVID-19 induced cytokine storm:
- Since COVID-19 virus is a small RNA virus, it has mutated several times and will keep mutating.
- A vaccine might not be able to prevent infection, but will definitely prevent COVID-19 induced cytokine storm (at least in majority of those vaccinated).
- Take ANY vaccine:
- All approved vaccines are more or less similar in terms of efficacy and safety.
- Don’t make the blunder of comparing efficacy of one vaccine from one study to efficacy of another vaccine from another study. Such comparison can be made only if the vaccines under question are compared with each other head to head in a single study. There are no such studies available (while I was writing this post). It is possible to find a vaccine with 60% efficacy in one study to be more efficacious than another vaccine with 90% efficacy in another study.
- It’s important to get vaccinated irrespective of what vaccine you take.
- Don’t test antibodies to check if vaccine is effective:
- After vaccination levels of antibodies will slowly come down with time. It doesn’t mean immunity is going away. You must remember that antibodies are targeted weapons- if there is no “target” virus, these antibodies are not needed.
- But, since you are vaccinated, your factory and production line are always there. Once the virus attacks, your adaptive immune system will just pick up activate the factory and pick up antibodies from there. Antibodies will rise from 0 to multifold like Phoenix rising from the ashes!
- Also, its very important to note that antibodies are just few amongst the several weapons prepared by our adaptive immune system once exposed to any vaccine. You cannot measure the cell mediated immunity (CMI) component of adaptive immunity by just measuring antibodies. And in case of viral infections, CMI is extremely critical. So, while antibodies indicate protection, lack of it doesn’t mean you have zero protection.
Coming Up:
In the next part (third part), we will explore how a healthy immune system prevents cytokine storm in majority of the patients with COVID-19 infection. We will also thoroughly investigate the defects in immune system of few people that make them unlucky enough to suffer from this horrific complication. This knowledge will complete the foundation necessary to answer our original question: “Who will require hospitalization in COVID-19?”




Very lucid presentation of very complex Immunolgy
subject..proud to be a student of Dr.Subir
Thank you for kind words Sureshji!
I have read your article carefully and I agree with you very much. This has provided a great help for my thesis writing, and I will seriously improve it. However, I don’t know much about a certain place. Can you help me?
I have read your article carefully and I agree with you very much. This has provided a great help for my thesis writing, and I will seriously improve it. However, I don’t know much about a certain place. Can you help me?